Note: This guideline is currently under review.
Introduction
Aim
Definition of Terms
Considerations
Management
Removal of Holter Monitor
Trouble shooting
Special Considerations
Links
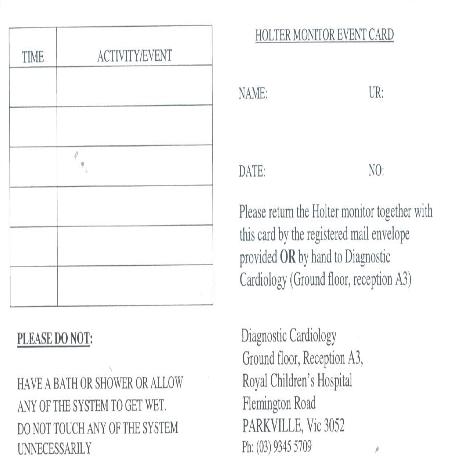
Appenix 1 - Holter Monitor Event Card
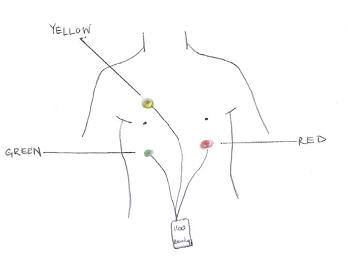
Appenix 2 - Placement of holter monitor electrode
References
Evidence Table
Introduction
A cardiac Holter monitor is a small, portable, non-invasive ambulatory device, used to record continuously the heart’s electrical activity in a 24–72 hour period. A cardiac Holter monitor is sometimes referred to as an ‘Ambulatory electrocardiography’ or ‘Ambulatory ECG’.
Cardiac Holter Monitors can provide the following information:
- Correlate any symptoms (chest pain, palpitations or syncope) the patient experiences with the heart’s electrical activity at that time;
- Record arrhythmias that occur, providing diagnostic information about the type of arrhythmia, how long it lasts, and what might trigger it;
- Determine the effectiveness of anti-arrhythmic medications.
The benefit of ambulatory ECG lies in its ability to examine continuously a patient over an extended period of time, permitting patient ambulatory activity while examining electrocardiographic activity in changing environmental situations (both physical and psychological).
Aim
To provide guidance on the management and troubleshooting of Holter Monitors. This clinical guideline applies to children requiring a Holter monitor during inpatient admission, children being discharged home with a Holter monitor and/or children having a Holter monitor applied during an outpatient clinic.
Definition of terms
- Cardiac Holter Monitor: Referred to in this clinical guideline as ‘Holter monitor’, is a small ambulatory, portable ECG device. Components include 3 electrodes and a Record Box.
- Record Box: The box records and stores continuous heart rhythm data transmitted by the electrodes. The Record Box will indicate it is working by displaying the time and a “recording” message on the screen.
- ECG – Electrocardiogram is a diagnostic tool that measures and records the electrical activity of the heart via electrodes placed on the skin.
- Event Card– Small booklet to highlight the time of Holter Monitor attachment and removal, and to record activities of the child while the Holter Monitor is attached.
- Arrhythmia – Irregular heart rhythm. Some common childhood arrhythmias include SVT, Long QT, Atrioventricular Heart Block, bradycardia, ectopic beats.
- Echo – Echocardiogram is an ultrasound test of the heart, helping to evaluate heart structure and blood flow.
Considerations for holter monitor
- A Holter Monitor will be attached to a child of any age, who, as per Cardiology team, requires further cardiac testing.
- Holter Monitor’s may be used in conjunction with other diagnostic tests, i.e. ECHO, 12-15 lead ECG, blood test and/or exercise stress test.
- The Cardiologist will determine the length of time the Holter Monitor should be left on.
- The Cardiology team will order the Holter Monitor on EMR. Nurses will be able to acknowledge the EMR Holter Monitor order in IP Summary and further view this order either in the EMR Chart Review Activity or ADT Navigator Activity.
- A Cardiac Technician is responsible for attaching the Holter Monitor.
- Prior to attaching the electrodes the skin must be clean, dry and hair free. The chest may be cleaned with normal saline/warm soapy water to remove any oily residue, or hair on the chest may need to be shaved, to ensure the electrodes stick well. Extra mefix tape may be secured over the electrodes to reinforce attachment.
- Holter Monitors may be attached within an inpatient or outpatient setting.
Management
- Once the Holter Monitor is attached to the patient it must stay on the patient for the prescribed time, 24-72hrs.
- For the inpatient with a Holter Monitor, nurses must document the time of attachment and the prescribed time to take off. Documentation of this information should occur in EMR Orders. The nurse should make the EMR order indicating time of attachment and time to take off.
- The Record Box should be checked once a shift to ensure the time and “recording” message is visible on the box.
- The child as an inpatient can have continuous cardiac monitoring by the bedside if clinically indicated while a Holter Monitor is attached.
- The child as an inpatient may leave the ward if clinically stable and approved by medical and nursing team.
- The child is allowed to go about normal activities of daily living, however they must avoid getting the Holter Monitor wet, therefore no showers or baths. It is also recommended to avoid the following: electric blankets and magnets. Signals from such devices may affect recording.
- Ensure the Record Box is in a carry pouch while the child is ambulating to ensure dots remain attached.
- Parents/Care givers should be encouraged to document activities in the
“Event’s Card” (see Appendix 1)
Removal of Holter Monitor
After the prescribed time, the Holter Monitor is removed from the child and, together with the Event’s record, returned to RCH Diagnostic Cardiology, Ground Floor, reception A3.
Returning Holter Monitor from home:
- Families are given a pre-stamped envelope with appropriate address to return Holter Monitor with Event’s Record to Diagnostic Cardiology
Returning Holter Monitor from inpatient ward:
- Holter Monitor and Event’s Card should be sent, via carps, to RCH Diagnostic Cardiology, Ground Floor, reception A3. Do not put Holter Monitor in pneumatic tube.
- In most cases the Cardiac Technician’s will go to the ward and remove the Holter Monitor from the patient close to the prescribed time.
- The cardiologist will analyse the Holter Monitor and organize follow-up with the child and family accordingly.
Troubleshooting
- Holter monitor electrodes fall off (see Appendix 2): It is important to reattach as soon as possible, and document the event in the Event’s Card.
- Record box is blank: Inform Cardiac Technician during working hours as it may need to be replaced. However if it is noticed after hours keep the dots on, document issue on Event’s Card and hand over so Cardiac Technicians can be informed during hours.
- Cardiac Technicians can be contacted on RCH extension 53902; otherwise contacting Cardiac Technician outside RCH call switchboard 9345 5522 and ask for “Cardiac Technician”.
Special considerations
Some children may experience minor skin irritation from the glue on the electrodes. If severe irritation occurs remove the dots and inform the cardiac team. It is rare that anaphylaxis will result, but perform skin, respiratory, circulatory and disability
assessment regularly to ensure child is stable. If anaphylaxis occurs employ
anaphylaxis guidelines.
Links
Clinical Practice Guidelines:
Anaphylaxis
Appendix 1 - Holter monitor event card
Appendix 2 - Placement of holter monitor electrode
References
- Czosek, R.J; Jefferies, J.L; Khoury, P.R; Anderson, J.B; Wilmot, I; Knilans, T.K & Spar, D.S (2016). Arrhythmic Burden and Ambulatory Monitoring of Pediatric Patients with Cardiomyopathy. PACE, 39: 443-451
- Follansbee, C.W; Beerman, L & Arora, G. (2018). Automated QT analysis on Holter monitors in pediatric patients can differentiate long QT syndrome from controls. Pacing Clinical Electrophysiology, 41: 50-56
- Hegazy, R.A & Lotfy, W.N. (2007) The Value of Holter Monitoring In The Assessment of Pediatric Patients. Indian Pacing and Electrophysiology Journal, 7(4):204-214
- Jacks, S.K; Kertesz, N.J; Witman, P.M & Faith, E.F (2015). Experience with Holter monitoring during propranolol therapy for infantile hemangiomas. Journal of American Academy of Dermatology, 73: 255-257.
- Reyes, E.V; Rizo, F.M; Santos, B.M; Jorge, J.G & Gonzalez, F.M (2010). Wireless communication interface for EEG/PSG Holter monitor. Journal of Medical Engineering & Technology, 34(3): 172-177.
- Uysal R, Bostan OM, Cetinkaya F, Deniz T, Cil E (2016). Syncope in Children: Is Rhythm Holter Monitoring Necessary? Journal of Current Pediatrics, 14: 124-128
- Yilmaz O, Ciftel M, Ozturk K, Kilic O, Kahveci H, Laloglu F, Ceylan O (2015). Assessment of heart rate variability in breath holding children by 24 hour Holter monitoring. Cardiology in the Young, 25: 317-323.
- http://www.melbourneheartcare.com.au/tests/24-hour-ambulatory-ecg-holter-monitoring/
- http://www.monashheart.org.au/content/Document/MonashHeart_Patient-Diary_Holter.pdf
- http://www.vcscardiology.com.au/index.php?option=com_content&view=article&id=59&Itemid=69
Evidence table
Click here to view the Holter Monitor guidleine's evidence table.
Please remember to read the
disclaimer.
The development of this nursing guideline was coordinated by Annabelle Santos, Clinical Support Nurse, Koala Ward, and approved by the Nursing Clinical Effectiveness Committee. Updated August 2020.