Introduction
Chemotherapy induced nausea and vomiting (CINV) is a common and extremely unpleasant side effect for children receiving antineoplastic therapy. CINV can lead to complications of treatment and cause significant emotional and physical distress, disruptions to
activities of daily living and influence the quality of life of the patient. The goal of antiemetic therapy is to prevent vomiting and minimise nausea before, during and after the administration of chemotherapy. The severity of nausea and vomiting can, to some degree, be predicted by the chemotherapeutic agents being
delivered but there is a degree of variation between patients. Antiemetic treatments should be initiated prior to the first dose of chemotherapy for best control of nausea and vomiting, as it can often become difficult to control nausea once the child is vomiting. Non-pharmacological measures are also an
important consideration and should be implemented in conjunction with pharmacological regimens to allow for the effective management of CINV.
Aim
The aim of this guideline is to provide an overview of the prevention and management of chemotherapy induced nausea and vomiting in the paediatric oncology patient.
Definition of terms
- Acute
CINV- CINV occurring within 24 hours of chemotherapy administration; peak intensity often occurs 5 to 6 hours after administration
- ALL- acute lymphoblastic leukemia
- AML- acute myeloid leukemia
- AUC- area under the curve (pharmacokinetics)
- Antineoplastic (anticancer)- therapy used to control or kill cancer cells; cytotoxic, hormonal, immunomodulatory, antiviral, biological and molecular targeted therapies may be used
- Anticipatory
CINV- CINV occurring within the
24 hour period prior to chemotherapy administration; often provoked by the environment or “thought” of chemotherapy (as example the sight of chemotherapy or when CVAD being accessed)
- BARF
scale- Baxter Animated Retching Faces scale (pictorial nausea scale)
- Breakthrough CINV- CINV occurring despite the use of preventative/prophylactic treatment; a failure to attain the goal of nil nausea and vomiting and a reasonable oral intake; often requires the use of other antiemetics; can be acute or delayed
- BSA- body surface area
- Chemotherapy- any chemical agent used to treat or control disease; most often used to describe treatment of malignant and other diseases with cytotoxic medicines
- CINV- chemotherapy induced nausea and vomiting; may be referred to as antineoplastic induced nausea and vomiting (AINV)
- CTZ- chemoreceptor trigger zone
- Delayed
CINV- CINV occurring 1-5 days after chemotherapy completion with a peak intensity 2-3 days post treatment completion; commonly associated with anthracyclines or platinum agents such as cisplatin or carboplatin
- Emesis- the action or process of vomiting
- Emetogenicity- likelihood of chemotherapy agent inducing nausea, vomiting or retching
- Haematopoietic
stem cell transplant (HSCT)- transplantation of the blood forming components/cells of the body
- HEC- highly emetogenic chemotherapy (or high emetogenic potential chemotherapy); greater than 90% frequency of emesis in the absence of effective prophylaxis
- LEC- low emetogenic chemotherapy (or low emetogenic potential chemotherapy); 10 to less than 30% frequency of emesis in the absence of effective prophylaxis
- MEC- moderate emetogenic chemotherapy (or moderate emetogenic potential chemotherapy); 30 to 90% frequency of emesis in the absence of effective prophylaxis
- MinEC- minimal emetogenic chemotherapy (or minimal emetogenic potential chemotherapy); less than 10% frequency of emesis in the absence of effective prophylaxis
- Nausea- an unpleasant feeling in the throat or stomach that may or may not result in vomiting
- NG- nasogastric
- Prophylaxis- prevention of
- Vomiting- ejecting part or all of the contents of the stomach through the mouth; emesis
- VAS- visual analogue scale
Assessment
All patients receiving chemotherapy for childhood cancer or as preconditioning for a haematopoietic stem cell transplant (HSCT) require ongoing assessment of the incidence and severity of nausea and vomiting.
It is the responsibility of nursing staff to regularly assess patients for signs and symptoms of CINV and decide on subsequent methods of management in consultation with the medical team and pharmacy.
The following assessment tools can assist in determining the incidence and severity of CINV. Results of the assessment tools should be clearly documented once per shift (more frequently if indicated) in the Electronic Medical Record (EMR). The CINV score (0 to 10) and type of scale
(BARF or VAS) utilized should be recorded under the Nausea Scale assessment in the Observation flowsheet.
Baxter
retching faces (BARF) nausea scale
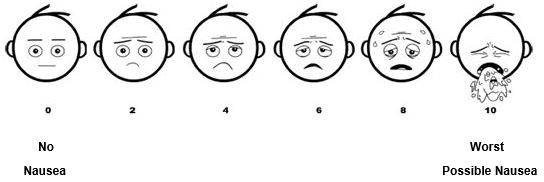
Visual Analogue Scale (VAS)
* Baxter Retching Faces Nausea Scale & Visual Analogue Scale- Baxter et al. (2011)
Each of the scales establishes a score from 0 to 10
- A score of 0 indicates no nausea
- A score of 10 indicates worst possible nausea
- The assessment tools should be utilised by health professionals to provide an overview of the child’s condition which will allow for an appropriate plan of care based on these findings.
Other
indications of children experiencing CINV may include
- Food refusal
- Decreased fluid intake
- Decreased urine output
- Retching
- Less interaction with others
- Sweating
Management
and principles of prevention and treatment of chemotherapy induced nausea and
vomiting
Emetic potential of chemotherapy agents
- Chemotherapy agents have different emetic potentials that are classified based on their risk of inducing nausea and vomiting.
Minimal
Emetogenic Potential (Minimal Emetogenic Chemotherapy or MinEC)
- Less than 10% frequency of emesis in the absence of effective prophylaxis
Low Emetogenic Potential
(Low Emetogenic Chemotherapy or LEC)
- 10 to less than 30% frequency of emesis in the absence of effective prophylaxis
Moderate
Emetogenic Potential (Moderate Emetogenic Chemotherapy or MEC)
- 30 to 90% frequency of emesis in the absence of effective prophylaxis
Highly
Emetogenic Potential (Highly Emetogenic Chemotherapy or HEC)
- Greater than 90% frequency of emesis in the absence of effective prophylaxis
Often, combinations of moderately emetogenic agents can yield a course with high emetic potential; for example, both ifosfamide and doxorubicin have moderate emetic potential yet when delivered together have high emetic potential. Other combinations of
chemotherapy can have low emetic potential but with extra antiemetic cover required at certain times; for example, ALL induction is generally minimal to low emetic potential but antiemetics are usually required around daunorubicin doses or on days when general anaesthetic has been given. The following provides an
outline of the emetic potential of common chemotherapy agents and regimens;
Guide to the emetic
potential of individual chemotherapy agents
Guide to the
emetic potential of combination chemotherapy regimens
Antiemetic treatments should be decided based on the emetic potential of the prescribed course of chemotherapy, although there may be some instances where a specific child requires deviations from the guidelines.
- Deviations from the guidelines should be discussed with the child’s Oncology Fellow/Consultant and Oncology Pharmacy.
- Once an effective antiemetic regimen has been determined for an individual child, this regimen should be used for future courses of chemotherapy as appropriate.
- Ensure details of a patient’s personalised antiemetic plan are documented by the Oncology Fellow/Consultant in the Antiemetic Plan tool located in the Oncology Activity in the EMR.
Pharmacological prevention and management of CINV
The goal of antiemetic therapy is to prevent vomiting and minimise nausea both during and after the administration of chemotherapy. For CINV prophylaxis to be effective;
- Antiemetics should be prescribed and released to the Medication Administration Record (MAR) from the Treatment Plan under the Oncology Activity on EMR
- Antiemetics appropriate for the emetogenic class of the chemotherapy agent or regimen, patient’s age and diagnosis should be
- administered regularly, regardless of nausea or vomiting status (this is to ensure the prevention of breakthrough and delayed CINV)
- continued throughout the period of administration of chemotherapy and for at least 24 hours following completion of chemotherapy
- Ensure antiemetics are ceased 24 to 48 hours following the completion of chemotherapy. Note: agents that cause delayed CINV may require antiemetics for up to 5 days following completion of chemotherapy. If antiemetics are required for longer, please discuss with the oncology fellow/consultant to exclude other causes of nausea and vomiting.
Antiemetic
medications
- The first dose of antiemetics should be given prior to commencing chemotherapy as per the following;
- Oral – 30 to 60 minutes prior to first dose of chemotherapy (optimal time is 60 minutes prior)
- Intravenous – immediately before or up to 30 minutes prior to first dose of chemotherapy (optimal time is 30 minutes prior)
Table one: Antiemetic medications
| Medication |
Dose |
Considerations |
|
Ondansetron
5HTз (serotonin) receptor antagonist
|
Oral/IV 0.15 mg/kg (maximum 8 mg) every 8 hours
Can be given every 6 hours (Paediatric Pharmacopoeia, 13th edition 2013*) with highly emetogenic chemotherapy. *RCH staff, please note: hardcopy available at the RCH library. |
IV administration; Refer to
Paediatric Injectable Guidelines
Efficacy is enhanced with Dexamethasone administration
Use in caution with patients with prolonged QT intervals: discuss the use of Ondansetron with fellow or consultant prior to prescribing. Consider concurrent administration of other medications that may prolong the QT interval, for example tyrosine kinase inhibitors (TKI) inhibitors such as Imatinib
and Sorafenib
Do not administer other 5HT3 antagonists concurrently with Ondansetron
First dose can be administered 12 hours after Granisetron (ensure Granisetron is ceased)
First dose can be administered 48 hours after Palonosetron (ensure Palonosetron is ceased) |
|
Palonosetron
5HTз (serotonin) receptor antagonist |
Administer as a single dose 30 to 60 minutes prior to the start of chemotherapy
One month to
< 17 years: IV 20 mcg/kg (maximum 250 mcg)
17 years and over: IV 250 mcg |
IV administration; Refer to
Paediatric Injectable Guidelines
Approved for use with
-highly emetogenic chemotherapy (HEC) where Dexamethasone and/or Fosaprepitant/Aprepitant is contraindicated
-moderately emetogenic chemotherapy (MEC) where Dexamethasone is contraindicated
-patients with prolonged QT intervals or those receiving concurrent administration of other medications that may prolong the QT interval, for example tyrosine kinase inhibitors (TKI) inhibitors such as Imatinib and Sorafenib
Do not administer other 5HT3 antagonists concurrently with Palonosetron
Patients may receive a second dose of Palonosetron at hour 48 of multiday chemotherapy regimens if clinically indicated, discuss with fellow or consultant
Requires DUC approval (Refer to
RCH Restricted Drug List)
|
|
Dexamethasone
Corticosteroid
|
Pre chemotherapy loading dose (used for HEC only)
BSA
< 0.6 m² : IV 4 mg
BSA 0.6 m² to
< 1.5 m² : IV 8 mg
BSA ≥ 1.5 m
² : IV 12 mg
Ongoing dose (start 12 hours after loading dose)
BSA
< 0.6 m² : Oral/IV 2 mg every 12 hours
BSA 0.6 m² to
< 1.5 m² : Oral/IV 4 mg every 12 hours
BSA ≥ 1.5 m
² : Oral/IV 6 mg every 12 hours
Maximum of 12 doses per course of chemotherapy |
If given concurrently with
Fosaprepitant or Aprepitant, reduce Dexamethasone dose by half
(Fosaprepitant/Aprepitant doubles the Area Under the Curve – AUC of
dexamethasone, which is a measure of exposure to dexamethasone)
IV administration; Refer to
Paediatric Injectable Guidelines
Not for use in children having chemotherapy for AML without direct fellow or consultant approval – may contribute to immunosuppression
Not for use in patients where corticosteroids are part of their chemotherapy regimen (B & T Cell ALL, NHL)
Not for use in children having chemotherapy for CNS tumours without direct fellow or consultant approval - may impair CNS penetration of chemotherapy
Not for use in patients receiving CAR T cell therapy without direct fellow or consultant approval – may impair CAR T cell activity
|
|
Fosaprepitant
Neurokinin-1 (NK-1) receptor antagonist |
≥ 6 months (and ≥ 6 kgs) to
< 2 years: IV 5 mg/kg as a single dose 30 to 60 minutes before chemotherapy on day 1
2 years to
< 12 years: IV 4 mg/kg (maximum 150 mg) as a single dose 30 to 60 minutes before chemotherapy on day 1
12 years and over: adult dosing, 150 mg as a single dose 30 to 60 minutes before chemotherapy on day 1 |
If Fosaprepitant given
concurrently with Dexamethasone, reduce the dose of Dexamethasone by half
(Fosaprepitant/Aprepitant doubles the Area Under the Curve – AUC of
dexamethasone, which is a measure of exposure to dexamethasone)
IV administration; Refer to
Paediatric Injectable Guidelines
Potent antiemetic reserved for highly emetogenic chemotherapy regimens or where breakthrough vomiting has occurred in past courses
Not for use in patients where corticosteroids are part of their chemotherapy treatment (B & T Cell ALL, NHL) without direct fellow or consultant approval
Use with caution in regimens that contain Ifosfamide due to increased risk of neurotoxicity
Patients may receive a second dose of Fosaprepitant at hour 72 of multiday chemotherapy regimens if clinically indicated, discuss with fellow or consultant
Requires DUC approval (Refer to
RCH Restricted Drug List)
|
Aprepitant
Neurokinin-1 (NK-1) receptor antagonist |
≥ 6 months (AND ≥ 6 kg) to
< 12 years:
Day 1: 1 hour prior to chemotherapy: 3 mg/kg (maximum 125 mg)
Day 2: 2 mg/kg/dose (maximum 80 mg)
Day 3: 2 mg/kg/dose (maximum 80 mg)
≥ 12 years (AND ≥ 30 kg):
Day 1: 1 hour prior to chemotherapy: 165 mg once within 72 hours |
If Aprepitant given concurrently
with Dexamethasone, reduce the dose of Dexamethasone by half (Fosaprepitant/Aprepitant
doubles the Area Under the Curve – AUC of dexamethasone, which is a measure
of exposure to dexamethasone)
Oral administration. Potent antiemetic reserved for highly emetogenic chemotherapy regimens or where breakthrough vomiting has occurred in past courses
Not for use in patients where corticosteroids are part of their chemotherapy treatment (B & T Cell ALL, NHL) without direct fellow or consultant approval
Use with caution in regimens that contain Ifosfamide due to increased risk of neurotoxicity
Course may be extended in some cases if required- discuss with fellow or consultant
Available through
Special Access Scheme and DUC approval (Refer to
RCH Restricted Drug List) |
|
Olanzapine
Dopamine receptor antagonist |
≥ 3 years to
< 17 years: Oral 0.1 mg/kg/dose (maximum 10 mg) once daily, round dose to nearest 1.25 mg
17 years and over: Oral 5 to 10 mg
once daily
Daily dose can be divided into twice daily dosing if required. |
Antipsychotic with antiemetic action, useful for breakthrough
vomiting
Monitor for dizziness, excess sedation and extrapyramidal
symptoms
Concomitant use of CNS depressants (e.g. opioids,
benzodiazepines, etc.) increases the risk of respiratory depression and
sedation
Do not use concurrently with Metoclopramide or Levomepromazine
May lower the seizure threshold, use cautiously in patients with
seizure history
No information for use in children younger than 3 years |
|
Levomepromazine
Dopamine receptor antagonist |
≥ 1 year to
< 12 years: Oral 0.25 mg/kg/day in 2 to 3 divided doses (maximum 40 mg/day)
≥ 12 years to
< 17 years: Oral 3 mg once or twice daily (dose may be increased as necessary and as tolerated to a maximum of 25 mg once or twice daily)
IV 0.05 mg/kg every 12 hours (maximum 25 mg daily), reduce dose by 50% if patient drowsy; if not sedated and still nauseous increase dose by 50% |
IV administration; Refer to
Paediatric Injectable Guidelines
Use in caution with patients with prolonged QT intervals: discuss the use of Levomepromazine with fellow or consultant prior to prescribing. Consider concurrent administration of other medications that may prolong the QT interval, for example tyrosine kinase inhibitors (TKI)
inhibitors such as Imatinib and Sorafenib.
Monitor for excess sedation and extrapyramidal symptoms
Concomitant use of CNS depressants (e.g., opioids, benzodiazepines etc.) increases the risk of respiratory depression and sedation
Do not use concurrently with Metoclopramide, Cyclizine or Olanzapine
May lower the seizure threshold, use cautiously in patients with seizure history
Not recommended for use in children
< 1 year due to increased risk of adverse effects
Available through
Special Access Scheme (Refer to
RCH Restricted Drug List) |
|
Metoclopramide
Dopamine receptor antagonist
|
Oral/IV 0.15 mg/kg (maximum 10 mg) every 8 hours
Total daily dose should not normally exceed 0.5 mg/kg |
IV administration; Refer to
Paediatric Injectable Guidelines
Discuss the use of Metoclopramide with fellow or consultant prior to prescribing
Monitor for extrapyramidal symptoms; acute dystonic reactions including oculogyric crises are rare, caution is advised for first exposure to Metoclopramide
If acute dystonic reaction occurs, administer
Benzatropine
Do not use concurrently with Olanzapine or Levomepromazine
May lower the seizure threshold, use cautiously in patients with seizure history
Not recommended for use in children
< 1 year |
|
Cyclizine
Antihistamine |
≥ 1 month to 18 years: oral/IV 0.5 to 1 mg/kg every 8 hours
<12 years: maximum 25 mg per dose
≥12 years: maximum 50 mg per dose |
IV administration; Refer to
Paediatric Injectable Guidelines
Rapid IV administration can cause drowsiness and dizziness, recommend administering over 30 minutes
Not a powerful antiemetic but may be used if vomiting persists despite recommended regimens
May antagonize the prokinetic effect of Metoclopramide – caution when used in combination
Not recommended for use in children
< 1 year due to increased risk of adverse effects |
|
Lorazepam
Benzodiazepine |
Oral 0.04 to 0.08 mg/kg/dose (maximum 2 mg per dose)
Administer once at bedtime the night before chemotherapy and once the next day prior to administration of chemotherapy. |
Little efficacy as antiemetic alone; not to be administered without additional antiemetics
Useful for anticipatory nausea and vomiting
Concomitant use of CNS depressants (e.g., opioids, benzodiazepines etc.) increases the risk of respiratory depression and sedation.
|
Antiemetic
Guideline
To ensure effective control of CINV, regular antiemetic therapy should be prescribed and administered according to the emetic potential of the chemotherapy agent or regimen. Recommended medications to be used as antiemetic therapy are outlined in the table below.
Antiemetic steroids should not
be used in patients with brain tumours, AML, CAR T cell therapy or patients
with corticosteroids as part of their chemotherapy regimen.
Halve dose of Dexamethasone if
using Fosaprepitant or Aprepitant.
Table two: Antiemetic guideline
| Age |
Minimal Emetogenicity
(MinEC) |
Low Emetogenicity
(LEC) |
Moderate Emetogenicity
(MEC) |
High Emetogenicity
(HEC) |
| Less than 6 months |
Regular
|
| Not required |
Ondansetron |
Ondansetron
Dexamethasone
If
Dexamethasone is contraindicated recommend:
Change Ondansetron to Palonosetron |
Ondansetron
Dexamethasone
Cyclizine
If
Dexamethasone is contraindicated recommend:
Change Ondansetron to Palonosetron |
| For
relief of breakthrough nausea and vomiting |
|
Step
1:
Escalate to LEC recommendations |
Step
1:
Optimise frequency of prescribed antiemetics
Step
2:
Escalate to MEC recommendations |
Step
1:
Optimise frequency of prescribed antiemetics
Step
2:
Escalate to HEC recommendations |
Step
1:
Optimise frequency of prescribed antiemetics
Step
2:
Change Ondansetron to Palonosetron |
| 6 months and over |
Regular
|
| Not required |
Ondansetron |
Ondansetron
Dexamethasone
If Dexamethasone
is contraindicated recommend:
Change Ondansetron to Palonosetron |
Ondansetron
Dexamethasone
Fosaprepitanta,b
If Dexamethasone
and/or Fosaprepitant is
contraindicated recommend:
Change Ondansetron to Palonosetron
Add Cyclizine |
| For
breakthrough or refractory nausea and vomiting |
|
Step
1:
Escalate to LEC recommendations |
Step
1:
Optimise frequency of prescribed antiemetics
Step
2:
Escalate to MEC recommendations |
Step
1:
Optimise frequency of prescribed antiemetics
Step
2:
Escalate to HEC recommendations |
Step
1:
Optimise frequency of prescribed antiemetics
Step
2:
Change Ondansetron to Palonosetron
Add Cyclizine
Step
3:
Consider adding Metoclopramide, Olanzapine or Levomepromazine
Note:
these medications interact, discuss with Oncology Consultant/ Fellow or Pharmacy
before prescribing |
a Aprepitant may be used instead of Fosaprepitant
b Omit Fosaprepitant/Aprepitant if known to interact with chemotherapy agent (monitor for signs of encephalopathy when used with Ifosfamide; anecdotal evidence in adults)
Adapted from the Royal Children’s Hospital, Melbourne (2014) & the National Child Cancer Network, New Zealand (2019)
Breakthrough
CINV
Breakthrough nausea and vomiting should be treated promptly. It is advised to have further antiemetics charted on the Treatment Plan under the Oncology Activity on EMR to enable nurses to initiate breakthrough medication as required.
Before prescribing further antiemetics, staff should review the Treatment Plan and contact the Oncology team to release any prescribed antiemetics to the MAR. The suggested order of escalation for breakthrough nausea and vomiting is outlined in the above table. This should be adjusted for individual situations.
Consideration should be given to the contribution of anticipatory nausea and vomiting which is likely to respond better to benzodiazepines and non-pharmacologic management.
Delayed CINV
This is defined as CINV occurring 1-5 days after chemotherapy and is most associated with anthracyclines or platinum agents such as Cisplatin or Carboplatin. Regular antiemetics should be continued for at least 48 hours after completion of Cisplatin
and in any other course of chemotherapy where delayed CINV has occurred in the past. Note: agents that cause delayed CINV may require antiemetics for up to 5 days following completion of chemotherapy.
Consideration may be given to a second dose of Fosaprepitant or a second dose of Palonosetron if this is appropriate. Ongoing Dexamethasone and Ondansetron may be sufficient.
Further
considerations
- Anticipatory CINV, is common in adolescents and rarely responds to standard antiemetic regimes. Benzodiazepines can be useful in this patient population but do not have direct antiemetic effects. The best treatment for anticipatory CINV is
prevention- if patients do not associate chemotherapy with nausea or vomiting, anticipatory CINV may not develop
- Dexamethasone should be charted regular (not PRN) if included in antiemetic regimes as the efficacy is enhanced with prophylactic administration
- Delayed CINV is common after chemotherapy courses containing Cisplatin. Antiemetics should be continued regularly for at least 48 hours after completing chemotherapy
- Ondansetron is as effective as Granisetron and is the 5HTз (serotonin) antagonist of choice for CINV. If Granisetron has been administered pre/post operatively, change antiemetic coverage to Ondansetron if child commencing chemotherapy (may commence administration of Ondansetron
12 hours post Granisetron; use in caution in patients with prolonged QT intervals or on multiple QT prolongating drugs, discuss with fellow or consultant prior to prescribing). Ensure Granisetron is ceased.
Non-pharmacological management of CINV
Despite the advances in pharmacological management, standard pharmacological regimes may not fully alleviate symptoms of CINV in paediatric oncology patients. Non-pharmacological interventions are an important consideration of antiemetic therapy. Non-pharmacological measures
should be implemented in conjunction with pharmacological regimes to allow for the effective management of CINV. The use of non-pharmacological measures may not be appropriate for each patient, interventions should be implemented according to the individual patient's needs and circumstances.
Music therapy and
relaxation
Music therapy and relaxation are beneficial interventions in managing CINV with minimal negative side effects. Music therapy may include a) live and active music engagement, and b) individual (recorded) music listening for refocusing and/or relaxation. These interventions are suitable for all ages,
are cost effective and can be implemented in the inpatient, outpatient and home environments. The music therapist is available to assess and advise on the most suitable plan for each patient.
Music listening/relaxation during chemotherapy:
- Where possible suggest to families to bring familiar music and music playing device for the first period of chemotherapy
- Involve a music therapist to assess the capability of children receiving chemotherapy to use music independently
- Encourage patients to listen to recorded music that is familiar and that they find comforting and relaxing during periods of chemotherapy (familiar music is the best option)
- For patients and families needing guidance the music therapist can make recommendations about styles of music that are effective in promoting relaxation for different age groups
- Commence music listening prior to chemotherapy administration or during experiences of anticipatory nausea and vomiting
- Contact Music Therapy, Educational Play Therapy or Comfort First Clinicians to assess if patient may benefit from focused breathing exercises to assist relaxation
- Encourage periods in a quiet environment
- Cluster medical and nursing care to allow for periods of rest
For children aged under 7 years, active music engagement may be more effective than passive music listening. The Music Therapist can advise/plan for this. See also section on Cognitive Distraction.
Guided imagery
Encouraging patients to focus on thoughts and images they find pleasing and relaxing will divert attention from nausea and vomiting to desirable thoughts and images.
- Encourage patients to visualise images related to the external environment (nature, landscape images) prior to and during chemotherapy administration
- Place appealing images/paintings in patients' rooms during chemotherapy administration
- Encourage patients to reside in areas where they can enjoy the outside view (e.g. by windows) during periods of nausea, vomiting and anxiety
- Implement music listening in combination with guided imagery for optimal management of nausea and vomiting
Cognitive
distraction
Cognitive distraction acts to counteract CINV by drawing a patient's attention away from feelings of nausea and vomiting and focusing attention on more pleasant activities. Patients should be encouraged to participate in
- Computer games
- Movies/Television
- Arts and crafts
- Developmental / Group play sessions
- Active Music Engagement
- Education sessions (kinder and school)
- Socialisation with family, friends and other patients
- Discussions about life outside of the hospital setting (pets, siblings, school, hobbies)
- Organising visits from volunteer services and ward grandparents available at the RCH
The Educational Play Therapy, Art Therapy and Music Therapy teams can assist in providing activities that promote cognitive refocussing to effectively manage CINV.
Massage
Educating families to perform massage during periods of chemotherapy has a positive impact on reducing levels of stress, anxiety, nausea and vomiting.
It is not recommended to
use massage for the paediatric oncology patient with a low platelet count
(platelets ≤ 20-30 x 10e9/L)
- Caution should be taken in patients receiving radiation. Avoid massaging areas that have received treatment to reduce irritation of irradiated skin and/or skin breakdown
- Caution should be taken in patients with solid tumours. Avoid massaging directly over areas where tumour is present to reduce associated pain and anxiety
- The level of pressure applied to the patient should be adjusted in those at risk of peripheral neuropathy
- Care should be taken to minimise massage movements that create a rocking motion in patients with nausea and vomiting
- Use non scented oils to reduce nausea associated with oil scents
- Care should be taken in patients with an accessed port (central venous access device) to avoid trauma
Acupressure
The acupressure technique involves the pressure applied to and then released from acupoints. Acupressure may be performed manually or with wrist pressure bands (also used for motion/travel sickness).
It is
not recommended to use acupressure for the paediatric oncology patient with a
low platelet count (platelets ≤ 20-30 x 10e9/L)
- Acupressure wrist bands may be applied to children prior to and during chemotherapy administration as tolerated
Manual
acupressure
- Perform daily during chemotherapy administration in the absence of acupressure wrist bands
- Pressure should be applied to acupoints for 1 to 3 minutes and then released
- Acupressure should commence prior to administration of chemotherapy and continue for the duration of the chemotherapy cycle
- Health professionals should familiarise themselves with the P6 acupressure technique. Adult studies have suggested pressure to the P6 acupoint may assist in the control of nausea and vomiting. The P6 acupoint is located on the inner forearm,
located 3 fingerbreadths below the wrist, between the two tendons.
- Encourage patients and families to familiarise themselves with the P6 acupressure point technique so they can independently perform this technique during treatment periods
Dietary
considerations
The following suggestions may be useful to help manage nausea and vomiting;
- Offer bland, dry foods such as toast and dry biscuits
- Offer smaller serves of food more frequently
- Offer sips of fluid throughout the day, sucking on ice cubes, fizzy drinks such as soda water or dry ginger ale and jellies can assist with an upset stomach
- Offer cold foods that have little smell
- Eat meals in a well ventilated room to clear the smell of foods away
- Encourage oral intake during times when the child feels less nauseated
- Discuss with your doctor/medical team about optimising anti-emetics
Enteral
nutrition (Nasogastric/PEG feeds)
- Consider reducing the rates of NG/PEG feeds during highly emetogenic chemotherapy
- If a child is vomiting during NG/PEG feeds, consider pausing the feeds for a short period (e.g. 1 hour) and restarting again at the last tolerated rate. If a child is on overnight NG/PEG feeds consider running total volume, prescribed by the dietitian, over 24 hours
- A dietitian can help to alter a child’s feeding regime if needed. Please refer to the dietitian for advice.
Other
considerations
- A multidisciplinary approach to managing CINV will assist in providing appropriate supportive care and effective antiemetic regimes to the paediatric oncology patient
- Current literature supports the use of ginger supplementation to manage general nausea and vomiting, however ginger is not recommended for use in the paediatric oncology population due to unknown effects on coagulation
- Poorly controlled CINV can result in dehydration, electrolyte imbalance, anorexia and fatigue
- Antiemetic therapies should be routinely administered during chemotherapy administration known to induce nausea and vomiting, not just PRN when patients develop symptoms of nausea
- If a patient is being discharged with antiemetic medications, the patient and/or caregivers should be given instructions on the management of antiemetic regimes at home prior to discharge
- The use of various forms of non-pharmacological and complementary therapies has also found to reduce nausea, vomiting and fatigue intensity, however should be discussed with the medical team prior to use
- Rinse the mouth thoroughly after
vomiting with water (stomach acid left in contact with the teeth and the
mouth lining will cause tooth decay and irritate the mouth)
Companion
documents
Information
for parents
Information
for Health Professionals
- Children’s Oncology Group (2022), Guidelines on Chemotherapy-induced Nausea and Vomiting in Pediatric Cancer Patients. COG Supportive Care Endorsed Guidelines, Children’s
Oncology Group (COG), Version date: July 15, 2022
- eviQ Clinical Resource; Prevention of antineoplastic induced nausea and vomiting
- Medicines information
- National Child Cancer Network New Zealand (2019), Clinical Guideline: Nausea and vomiting - chemotherapy and radiotherapy induced: prevention and treatment, Version date: 12 August, 2019
Evidence table
The evidence table for this guideline can be found here.
Please remember to read the
disclaimer.
The development of this nursing guideline was coordinated by Lisa Barrow, CNE, Kookaburra, and approved by the Nursing Clinical Effectiveness Committee. Updated May 2023.