What are dietary therapies for epilepsy?
Ketogenic diets are strict, medically supervised diets that may be a treatment option for some infants and children with epilepsy. They involve a high fat and very low carbohydrate diet that ensures the body will mainly burn fat rather than carbohydrate and protein for energy, thus producing
ketones. The brain can use ketones as an alternative source of energy. In some ways, the diet mimics the body’s metabolic state during fasting or illness. This high ketone state (ketosis) decreases seizure activity in some circumstances by mechanisms which are not fully understood. The diet
deliberately maintains this high level of ketones by a strictly calculated, individual regimen with rigid meal plans.
There are two types of ketogenic diet therapies offered at The Royal Children’s Hospital; the Classical Ketogenic Diet (CKD) which is very low in carbohydrates, adequate in protein and high in fat and the Modified Atkins Diet (MAD) which is low in carbohydrates, moderate in protein and high in fat. These
differ from the ‘keto’ diet that is popular on social media.
A ketogenic diet is not a "natural therapy". All diet therapies for epilepsy must be medically supervised, requiring regular monitoring to help prevent potential side effects; that may include nutritional deficiencies, poor growth, kidney stones, high cholesterol and others.
Who is the diet for?
Ketogenic diets are generally only suitable for children with seizures that are poorly controlled with medication or those with Glucose Transporter Type 1 Deficiency Syndrome (GLUT 1 deficiency). Assessment by a paediatric neurologist experienced in epilepsy management is a prerequisite. Generally,
children with myoclonic-atonic seizures, infantile spasms, Dravet syndrome and absence seizures are thought to respond best to the ketogenic diet.
What is involved prior to commencing the ketogenic diet?
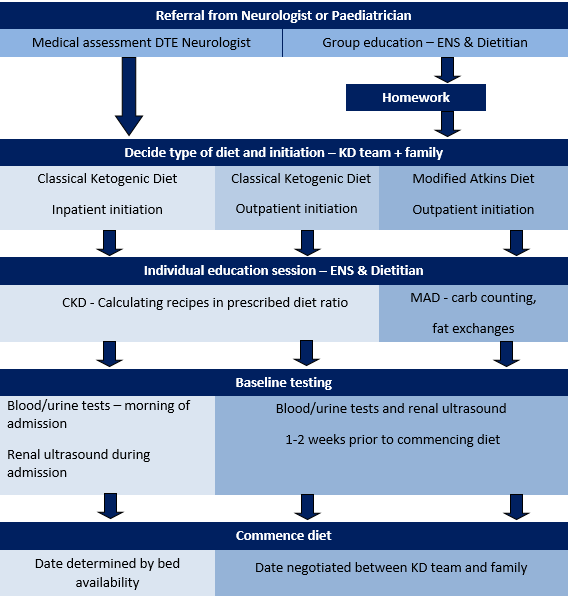
All children require a referral from their neurologist or paediatrician to the Dietary Therapies for Epilipsy (DTE) Clinic for assessment of their suitability for treatment. A thorough assessment takes place which includes a medical assessment of the patient, baseline investigations, group education session
with the epilepsy nurse specialist (ENS) and dietitian, homework tasks and individual education sessions. The process is outlined below.
How is a ketogenic diet commenced?
Ketogenic diets can be commenced either in hospital, or at home. The location will depend on the type of diet, the child’s age and medical stability.
Inpatient initiation
Classical Ketogenic Diet
Children are admitted on a Monday to the Cockatoo (neurology) ward following fasting blood and urine tests and an ECG. The length of admission is 4-5 days. During the admission children will be required to drink a ketogenic formula called KetoCalTM for 48 hours before progressing
to special ketogenic meals which are prepared in the hospital kitchen. During the admission close monitoring of blood ketones and blood glucose levels will occur. The Ketogenic Diet Team will review the child daily during admission.
Outpatient initiation
Classical Ketogenic Diet (CKD) or Modified Atkins Diet (MAD)
The timing of outpatient initiation is negotiated between the Ketogenic Diet Team and the family. It is usually recommended that the diet be commenced on a Monday and it usually takes around 2 weeks to get to the target diet for the CKD and 5 days for the MAD. Prior to this time
investigations such as renal ultrasound, fasting blood and urine tests and growth measurements will be taken at the hospital. During home initiation, food is commenced from day 1. For the CKD, blood ketone and blood glucose monitoring is completed three times per day by a family member. For the MAD, urine ketones
are commenced twice daily. The epilepsy nurse and dietitian will contact you daily to review initially.
For both the CKD and the MAD your child’s medications will need to be changed to tablet form but their doses will continue as normal. They are encouraged to maintain normal activities and are not confined to bed rest.
How likely is the diet to work?
It is important to have realistic expectations about the likelihood of dietary therapy helping your child’s epilepsy. The ketogenic diet does not control seizures in all children. In fact, only a relatively small proportion of children benefit significantly from the ketogenic diet. If all types of epilepsy are considered, just over one
in three children will have more than a 50% reduction in their seizure frequency. Another one in three will have less than a 50% reduction in seizure frequency and the remaining one in three will have no change in seizure frequency. Less than one in ten will have more than a 90% reduction in seizures
and less than one in twenty will become seizure free.
However, some forms of epilepsy may respond better, such as absence epilepsy, myoclonic-atonic epilepsy (Doose syndrome), Dravet syndrome and infantile spasms. For example, small studies suggest that more than two thirds of these children will halve more than halving of their
seizures, and one-fifth to one-third of children will become seizure free.
There is limited information to determine whether the CKD is more effective than the MAD but the CKD is usually considered to be “gold standard” dietary treatment.
What does it look like?
Classical ketogenic diet
The dietitian will calculate the amount of calories and protein that your child will need to ensure adequate growth and determine the correct diet ratio of fat to carbohydrates and protein to ensure ketosis. Parents are encouraged to learn how to calculate ketogenic recipes and
the dietitian will provide education. Ketogenic recipes will be different to ‘normal’ recipes as they are very high in fat and very low in carbohydrates. Foods such as bread, pasta, rice and potatoes are generally not allowed. The meal plan is usually divided into three meals and two snacks per day. Eating
‘extra’ foods outside the meal plan is not allowed. Meals tend to be smaller than normal due to the high fat content. Water is the main fluid allowed. As the diet is nutritionally inadequate daily vitamin and mineral supplements are necessary.



Modified Atkins diet
The MAD is calculated in a different way from the CKD. Carbohydrates are strictly counted and fat serves are added to meals but protein and diet ratios are not counted. Foods such as bread, pasta, rice and potatoes are generally not permitted, however protein foods
such as meat, eggs and cheese are allowed to appetite. Parents are encouraged to learn how to calculate MAD recipes and the dietitian will provide education. Water is the main fluid allowed. As the diet is nutritionally inadequate daily vitamin and mineral supplements are necessary.

What is required at home?
Basic equipment for home includes:
- Electronic weigh scales accurate to 1 gram
- Measuring cups and spoons (Modified Atkins Diet)
- Silicone spatula
- Vitamin and mineral supplements as advised by the dietitian
- Ketone monitoring equipment
- Computer access with Microsoft Excel program (Classical Ketogenic Diet)
A ketogenic diet must be strictly followed at all times. Children attending play group, kindergarten, school or social occasions must take the required meal with them. All carers and teachers must be fully informed of the diet. Families initially find planning and preparing
the diet very time consuming, but with practice this becomes easier and faster. Shopping practices change, but costs are comparable to normal household budgets. The initial outlay for necessary equipment may be a cost factor.
What problems can arise?
Loss of ketosis may occur in some children on the ketogenic diet for reasons including:
- the child is given food that is not on the ketogenic diet or is secretly eating extra food
- incorrect calculation and preparation of food
- the child is unwell
- incorrect nutritional content documented on food product labels
- medication given that contains too much carbohydrate
Constipation can occur because of the small volume of food and fibre consumed. This is managed with increasing fluid intake and the use of a laxative such as MovicolTM
Weight loss or gain. This is managed by adjusting the energy intake.
Height slowing (stunting).
Inappropriate food related behaviours such as refusal of certain foods.
Compliance of children may be an issue especially in some social circumstances.
Less common and potentially more serious long term side effects, which are monitored and screened for as part of regular reviews include:
- Kidney stones have been described in 3-7% of children. This problem can be decreased by regular urine monitoring.
- Bone health may require increase monitoring with bone scans.
- High cholesterol. The long-term outcomes of a high fat diet are not yet known.
Links
Epilepsy Foundation
Epilepsy Queensland
Charlie Foundation
Matthew’s Friends
References
Books
The Ketogenic and Modified Atkins Diets: Treatment for epilepsy and other disorders. 6th Edition 2016. Eric H Kossofff, Zagava Tunrer, Sarah Doerrer, Mackenzie C. Cercenka Bobby J Henry. Demos Health.
Ketocooking: A practical guide to the ketogenic diet. 2012 Judy Nation, J. Helen Cross, Ingrid E. Scheffer. The Homewood Press
Journal
Articles
Kossoff, EH, et al. Optimal clinical management of children receiving dietary therapies for epilepsy: Updated recommendations of the International Ketogenic Diet Study Group. Epilepsia Open 2018;3(2):175-192
van der Louw, E, et al. Ketogenic diet guidelines for infants with refractory epilepsy. European Journal of Paediatric Neurology 2016;20(6):798-809