To feed well, babies need to position their lips and tongue around the nipple or artificial teat, and create both suction and compression during sucking.
Sucking is more difficult when a baby is born with a cleft palate or combined cleft lip and cleft palate. There are a number of ways to help these babies feed well, including the use of specially designed bottles and teats.
To learn more about cleft lip and cleft palate, read our fact sheet
Cleft lip and cleft palate.
Feeding your baby
Your cleft coordinator, speech pathologist or Maternal and Child Health Nurse will be able to help show you what it should look like when your baby is feeding properly. Signs that your baby is feeding well are that they have five or six wet nappies per day, regular bowel motions and they are
healthy and alert.
Feeding with a cleft lip
Babies born with a cleft lip alone usually feed well. Some babies breastfeed better with the cleft facing upwards. The breast tissue usually fills the gap where the cleft is and allows efficient feeding. Some bottle-fed babies feed better on a wide-based teat.
Feeding with a cleft palate
Babies with cleft palate often look like they are feeding well, because the lips and tongue close around the nipple or artificial teat like non-cleft babies and the jaw moves well during sucking.
However, most babies with cleft palate cannot generate suction during feeding. This is because air leaks from the mouth through the cleft into the nose during feeding. The lack of suction makes it difficult – and for some babies, impossible – to breastfeed or drink from a bottle
efficiently. This means that feeding can take a long time and is tiring for your baby, who may not get enough milk to grow and develop well.
Feeding with a cleft lip and palate
Babies with cleft palate can't create enough suction during feeding to draw milk from the breast or bottle easily. If your baby also has a cleft lip, they may not be able to compress the breast or teat well enough to push milk from the breast or bottle. In either case, feeding is usually slow
and tiring, and your baby may not drink enough to grow well.
Feeding options
Breastfeeding
If your baby can't feed well directly from the breast, you may choose to feed your baby expressed breastmilk (EBM) from a bottle. Lactation consultants and Maternal and Child Health Nurses are able to provide advice and support to new mothers who wish to express
breastmilk for their baby.
Bottle feeding
For babies with a cleft lip only, there is no need to use special equipment if your baby feeds well from a standard teat or bottle bought from a supermarket or pharmacy. But if your baby has a cleft palate or cleft lip and palate they generally cannot generate suction and/or compression during feeding, therefore they will need a specialised cleft bottle to feed. There are a number of special teats and bottles available. Bottles and
teats that can be squeezed while your baby is sucking compensates for a lack of suction.
Your cleft coordinator can show you the different bottles and teats available and demonstrate how to use them. Some commonly used teats and bottles include:
- The SpecialNeeds® Feeder: Previously known as the Haberman feeder, this has a long narrow teat which is squeezed during feeding to release milk into the baby's mouth. The teat has a 'slit' cut and allows slow, medium or fast flow depending on the orientation of the slit during
feeding. The teat also has a one-way valve to minimise swallowing of air, and maximise response to compression.
- Dr Brown's Specialised Feeding System: The Dr Brown bottle has three critical elements
to ensure the functionality of the speciality feeding system. A one way infant
paced feeding valve. Internal vent system creating the vacuum-free feeding
experience. Consistent and reliable teat flow rates. Unique one way valve means
no manual assistance is required for feeding.
- Queensland CleftPALS Bottle: This is a soft polythene bottle made by Queensland CleftPALS Inc. It works well with a number of different teats and is gently squeezed during feeding to assist the baby in receiving milk.
- Pigeon Cleft Teat: This is an isoprene rubber teat that can be used with a squeeze bottle or a normal rigid bottle. It comes with a plastic regulator that can be inserted into the teat to assist with milk flow. The thicker part of the teat must be facing upwards (towards the roof of
the mouth) for efficient feeding.
- Chu Chu Easy Feed Teat: This is a silicone rubber teat (nitrosamine free), that can be used with a squeeze bottle or normal bottle. When feeding, ensure the flat part of the teat is facing upwards (towards the roof of the mouth).
- Chu Chu Cross-cut Teat: This is an isoprene rubber teat (nitrosamine free) that can be used with a squeeze bottle or normal bottle. It has a cross-cut in the top, which stops milk dripping into the baby's mouth when they have stopped for a rest during a feed.
See the end of this fact sheet for details on where to get these teats and bottles.
Feeding tips
Each baby is unique, so different techniques will suit different babies, even if they have the same kind of cleft. However, some general tips are:
- Feed your baby in a calm quiet environment. Make sure you are sitting in a comfortable chair.
- Have several breaks for burping, as your baby may experience a lot of wind.
- Keep each feed to 20–30 minutes. Longer feeds mean your baby will use too much energy during feeding.
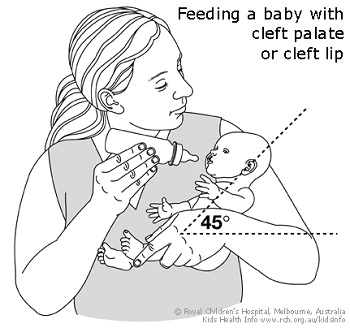
- Seat your baby fairly upright for bottle feeding (see diagram below). This may prevent milk coming out of your baby's nose during sucking. Hold your baby close to you so they are well supported during feeding.
- If your baby has a cleft lip, avoid placing the teat into the cleft.
- Once your baby starts sucking, squeeze the bottle gently to deliver milk into the mouth. If you are using the SpecialNeeds Feeder, the teat rather than the bottle should be squeezed. A squeeze every three to four sucks is usually enough.
- Some parents find it helpful to practise squeezing a water-filled bottle to get an idea of how the flow changes with more rapid squeezing or stronger squeezing of the bottle.
- Watch how your baby reacts to the pulsing or prolonged squeezing of the bottle. If they look uncomfortable or are not managing the mouthful of milk, stop squeezing and let your baby rest and swallow before more milk is given.
- Some babies have serious feeding problems (dysphagia), which mean they need specialised help to manage feeding. If your baby is showing signs of swallowing difficulties, talk to your child's doctor or cleft coordinator.
Introducing solids
Babies with cleft lip, cleft palate or cleft lip and palate usually start taking solids at the same time as other babies (between four to six months of age).
Sometimes food may come out through your baby's nose during feeding. This may improve if you sit your baby more upright or make the food a little runnier. If problems persist, you can contact your speech pathologist for advice.
Feeding your baby after cleft lip or cleft palate repair
Your plastic surgeon will give specific instructions on how to feed your child in the first few days after the surgery. In general, babies are encouraged to return to their usual method of feeding (breastfeeding or bottle feeding) after surgery. If the baby has progressed to solids,
these can also be reintroduced quite quickly after palate repair surgery. The food should be a soft, sloppy consistency for the first three weeks.
For more information
Where to get equipment
You can get specialist bottles and teats from:
Common questions our doctors are asked
How do I know if my baby is not feeding properly?
Newborn babies can lose up to 10 per cent of their birth weight, but usually regain it in two to three weeks. If your baby is having five or six wet nappies per day, regular bowel motions and is healthy and alert, then it is likely that they are feeding well. Slow weight gain or
weight loss may mean the feeding method needs to be changed. If you are worried about your baby's feeding, talk to your GP, cleft coordinator or Maternal Child and Health Nurse.
Developed by The Royal Children's Hospital Speech Pathology and Plastic and Maxillofacial Surgery departments. We acknowledge the input of RCH consumers and carers.
Reviewed August 2020.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit
www.rchfoundation.org.au.