Physeal anatomy
The key difference between the child's bone and that of an adult is the presence of a physis. Physeal injuries are very common in children, making up 15-30% of all bony injuries.
The growth plate, or physis, is the translucent, cartilaginous disc separating the epiphysis from the metaphysis and is responsible for longitudinal growth of long bones.
The cells of the physis are arranged in columns or layers described as the germinal or resting layer, the proliferative zone, the hypertrophic zone and the zone of provisional calcification (Figure 10). The proliferative zone is where the chondrocytes undergo rapid division by mitosis and is the most metabolically active zone. Osteoblasts use the chondrocyte columns as a scaffold for ossification in the zone of provisional calcification. The hypertrophic zone is the weakest because it lacks both collagen and calcified tissue. Most physeal separations occur through this layer because it is less able to resist shearing stress.
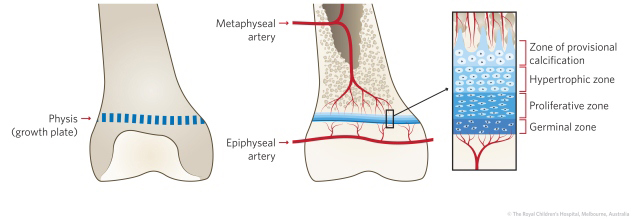
Figure 10: Anatomy of the physis (growth plate).
|
The macroscopic structure of the growth plates varies according to the degree of stress to which it is exposed. Around the knee, the stresses are high and in order to resist shear, the physis interdigitates with surrounding bone in what are known as mammillary bodies. This anatomic arrangement locks the physis solidly. If it does sustain a shear injury there is a higher chance of developing a bony bar across the physis and subsequent growth arrest. This is in contrast to the commonly injured distal radial physis that is more linear and rarely arrests.
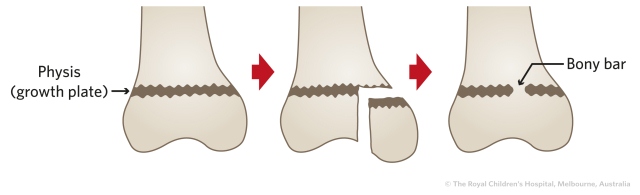
Figure 11: The undulating shape of the distal femoral physis and the presence of mamimillary bodies provides extra stability to the growth plate. However, due to this anatomy, there is a higher chance of a growth arrest to occur following injury.
Salter-Harris classification of physeal injuries
Although there are more recent and more complex classifications, the Salter-Harris classification is the most widely used and clinically useful approach to classifying and describing physeal injuries in children. About 90% of children with physeal injuries can be classified using the five Salter-Harris classifications from plain x-rays (Table 1). Another 5% can be classified using one of the more elaborate systems and the final 5% defy classification. When an apparently "unclassifiable pattern" is encountered, additional imaging may be helpful, including oblique views, an arthrogram, CT or MRI.
Table 1: Salter-Harris classification of physeal injuries.
| Type |
X-ray |
Description |
|
|
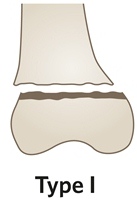
Accounts for 6% of all physeal injuries.
Transverse fracture through the growth plate.
In a type I separation, the epiphysis separates from the metaphysis. The plane of separation is horizontal and the germinal cells remain with the epiphysis.
When the periosteum is torn, displacement may occur. The periosteum is usually torn on the convex side and is intact on the concave side. Displacement is usually easily reduced by reversing the deforming forces and these are often stable and treated by closed means.
When the periosteum is not torn, there is no displacement and these injuries are diagnosed by suspicion, by the sign of local tenderness and by the normal appearance on x-ray. They are usually misdiagnosed as sprains because little is seen on the x-ray.
Healing is rapid for type I fractures, within 2-3 weeks of injury and problems are rare especially in sites such as the distal radius.
|
|
 |
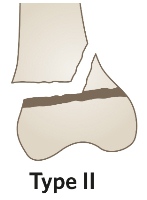
Most common type and accounts for 75% of all physeal injuries.
Transverse fracture through the growth plate and an oblique or vertical fracture through the metaphysis.
The type II injury starts as a horizontal separation (like type I) but this is completed by exiting through the metaphysis, resulting in a triangular fragment which varies in size.
This is the most common type of physeal separation and is usually easily reduced but not always easy to hold reduced, in a cast. Sometimes the torn periosteum becomes trapped in the fracture site preventing a full reduction by closed means. The trapped periosteum sometimes needs to be released by open operation, especially at the ankle.
|

|
 |
Accounts for 8% of all physeal injuries.
Transverse fracture through the growth plate and a vertical fracture through the epiphysis.
Type III injuries are more commonly seen in older children where the growth plates have started to close. It is a combination of a horizontal fracture line through the physis and a vertical fracture line which runs from the growth plate through the epiphysis to the articular surface.
Displaced injuries may result in a physeal bar, leading to growth disturbance and joint incongruity, leading to arthritis. Most displaced type III injuries require open reduction internal fixation (ORIF).
|
|
 |
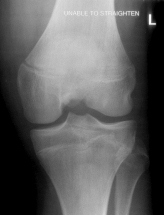
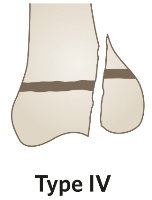
Accounts for 10% of all physeal injuries.
Vertical fracture through all three components, metaphysis, physis and epiphysis.
In type IV separations, the fracture line is vertical. It extends through four distinct tissues/areas: metaphyseal bone, physeal cartilage, epiphyseal bone or cartilage and articular cartilage. The most common example of a type IV physeal injury is separation of the lateral condyle of the distal humerus. The four injured tissues must be accurately reduced and lined up with each other, to minimise the risk of a physeal bar and articular incongruity. Most displaced type IV injuries require ORIF and long-term follow-up to detect growth disturbance.
|
 |
|
This injury is rare and difficult to see on x-ray.
Compression fracture or crushing of the growth plate.
These injuries are almost always diagnosed retrospectively, when a growth arrest has occurred.
|
Management of physeal injuries
- Look for and define the exact lines of separation on good quality x-rays using multiple views
- Occasionally views of the opposite side may help
- Classify the injury using the Salter-Harris classification
- If not readily classifiable, consider CT, MRI and urgent referral to orthopaedics
- The majority of type I and II injuries are treated by closed reduction and cast immobilisation
- The majority of type III and IV injuries require ORIF
Physeal injuries become "sticky" and unite very quickly, in good position or in bad. They should not be referred to "next available clinic" but reduced in ED or by orthopaedics within 24 hours of presentation (Figure 12). Reduction should therefore be early and gentle, so that iatrogenic trauma is not added to the original trauma. If an acceptable reduction is not possible at the first attempt, referral for open reduction should be considered promptly.
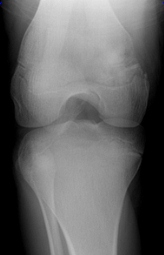
Figure 12: A. AP and lateral x-ray demonstrating a Salter-Harris type II fracture. B. This fracture underwent closed reduction.
The majority of type I and II injuries should not have attempted manipulation after 5 days. Most will remodel and the rest can be managed by osteotomy. The situation is more complex with type III and type IV injuries. ORIF may be considered for many weeks after injury but outcomes become exponentially worse with time (Figure 13).
 |
 |
A
|
B
|
Figure 13: A. AP x-ray of a Salter-Harris type IV distal tibia fracture. B. This was internally fixated with a cannulated screw, restoring joint congruence and anatomy of the physis.
Open versus closed reduction
Type I and type II injuries are common at the wrist, ankle, knee and shoulder. An exact anatomic reduction is not essential at the wrist or shoulder because remodelling will take care of minor degrees of displacement. Accurate reduction is more critical at the ankle and knee.
Type III and type IV injuries involve the joint surface and an anatomic reduction is mandatory. These injuries require prompt referral, accurate reduction and usually some form of fixation, either percutaneous or open fixation.
Complications
The majority of physeal injuries heal quickly and recover fully. In a minority, growth disturbance or arrest may occur, and can result in deformity and impaired function.
Physeal growth may be disturbed by:
- Avascular necrosis
- Direct crushing (Salter-Harris type V)
- The formation of a bony bar
- Non-union
- Hyperaemia