Fracture Guideline Index
See also:
Tibial shaft (diaphyseal) fracture - Fracture clinics
- Summary
- How are they classified?
- How common are they and how do they occur?
- What do they look like - clinically?
- What is a toddler's fracture?
- What radiological investigations should be ordered?
- What do they look like on x-ray?
- When is reduction (non-operative and operative) required?
- Do I need to refer to orthopaedics now?
- What is the usual ED management for this injury?
- What follow-up is required?
- What advice should I give to parents?
- What are the potential complications associated with this injury?
1. Summary
Fracture type
|
ED management
|
Follow-up
|
Toddler fracture
|
Treatment is supportive. A backslab can be applied. An above-knee walking cast for 4 weeks is optional
|
Fracture clinic in 2 weeks with x-ray
|
Undisplaced tibial shaft fracture
|
No reduction is needed. Above-knee cast for 4-6 weeks (age and healing-dependent)
Patient would benefit from procedural sedation for application of the cast
|
Fracture clinic in 1 week with x-ray
|
Displaced tibial shaft fracture + / - fibular shaft fracture
|
See acceptable reduction parameters
Closed reduction with above-knee cast for 4-6 weeks (age and healing-dependent), non-weight bearing
Unstable fractures may require general anaesthesic, manipulation and plaster GAMP) or fixation in theatre
|
Fracture clinic in 1 week with x-ray
|
2. How are they classified?
Tibial shaft (diaphyseal) fractures can be classified by:
a). location - proximal, middle, or distal third
b). fracture pattern - transverse, spiral/oblique, comminuted or open
c). involvement of the fibula
3. How common are they and how do they occur?
Tibial shaft fractures are the third most common long bone fracture in children and adolescents.
Fractures of the shaft of the tibia can result from a direct blow or a rotational force. Direct trauma frequently produces a transverse fracture or segmental fracture pattern, whereas rotational forces typically result in an oblique or spiral fracture.
!
|
Thirty percent of tibial shaft fractures are associated with a fibula fracture
|
4. What do they look like - clinically?
The child will present with pain, swelling and/or deformity in the lower leg. The child will not want to weight bear on the injured leg.
5. What is a toddler fracture?
Toddler fractures occur in young ambulatory children (from 9 months to 3 years). A toddler's fracture is a spiral or oblique undisplaced fracture of the distal shaft of the tibia with an intact fibula. The periosteum remains intact and the bone is stable. These fractures occur as a result of a twisting injury. Septic arthritis and osteomyelitis should be excluded.
6. What radiological investigations should be ordered?
Anteroposterior (AP) and lateral x-rays of the tibia and fibula to include knee and ankle joints should be ordered.
7. What do they look like on x-ray?




A B
Figure 1: Toddler fractures are often radiographically normal on initial x-ray. A) AP and lateral x-ray of a 15 month old boy who refused to weight bear. No fracture can be seen. When routine radiographs are normal but a fracture is suspected, oblique views may help visualise the fracture line. B)Radiographic evidence may only become apparent 7-10 days after the initial injury when new periosteal bone formation occurs (white arrow).
- Undisplaced complete isolated fracture of tibial shaft


Figure 2: Undisplaced complete isolated fracture of the tibial shaft. Most tibial shaft fractures are short oblique or transverse fractures of the middle or distal third.
- Displaced fracture of the tibial shaft
.jpg)
Figure 3: With an intact fibula it will tend to push the tibia into varus during healing. Thus when casting this fracture the cast should be moulded into slight valgus to protect against this.
- Tibia and fibula fracture

Figure 4: AP and lateral x-ray of tibia and fibula shaft. The tibial shaft fracture is located in the distal third. The fibula fracture is located in the proximal third.
8. When is reduction (non-operative and operative) required?
Reduction is required with any displaced fracture. The majority will require closed reduction.
AP and lateral radiographs of the tibia, including the knee and ankle joints should be obtained immediately after reduction to verify alignment.
Table 1: Acceptable reduction parameters.
Parameter
|
<8 years
|
>8 years
|
AP or lateral x-ray
|
10 degrees
|
5 degrees
|
Shortening
|
10 mm
|
5 mm
|
Rotation
|
10 degrees
|
5 degrees
|
Apposition
|
0%
|
50%
|
9. Do I need to refer to orthopaedics now?
Indications for prompt consultation include:
- open fractures
- extreme swelling/compartment syndrome
- neurovascular injury with fracture
- unable to achieve or maintain reduction (including if ED is not experienced in fracture reduction, splinting or casting)
- ipsilateral leg injuries
10. What is the usual ED management for this injury?
Fracture type
|
Type of reduction
|
Immobilisation method and duration
|
Toddler fracture
|
No reduction is needed
|
Treatment is supportive. A backslab can be applied. An above-knee walking cast for 4 weeks is optional
|
Undisplaced tibial shaft fracture
|
No reduction is needed, however the patient would benefit from procedural sedation for application of the cast
|
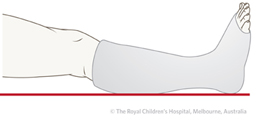
Above-knee cast for 4-6 weeks (age-and healing-dependent), non-weight bearing. Above-knee cast should typically have the knee flexed to 30-40 degrees and the ankle in neutral dorsiflexion
Change to patellar tendon-bearing/below-knee cast
Patella tendon-bearing cast

Below-knee cast
|
Displaced tibial shaft fracture + / - fibular shaft fracture
|
Closed reduction
Unstable fractures may require general anaesthetic, manipulation and plaster (GAMP) or fixation in theatre
|
Above-knee cast for 4-6 weeks (age-and healing-dependent), non-weight bearing. Above-knee cast should typically have the knee flexed to 30-40 degrees and the ankle in neutral dorsiflexion
Change to patellar tendon-bearing/below-knee cast
|
11. What follow-up is required?
Patients who have undergone a closed reduction and casting need follow-up in 1 week in the fracture clinic with an x-ray.
12. What advice should I give to parents?
Most fractures will heal well without complication in 8-12 weeks. Close follow-up is important to monitor fracture alignment.
Parents and the child should be given education on cast care. Give "Caring for your child in a leg cast" fact sheet.
13. What are the potential complications associated with this injury?
- Compartment syndrome - soft tissue swelling and circumferential casting can lead to an acute compartment syndrome. Signs and symptoms include increasing pain, pain on passive stretch of the toes, swelling and late signs of circulation compromise. Injuries with concerning swelling should be splinted and have delayed casting to let the swelling reduce. Close observation and clinical monitoring needs to be done for patients with high energy injuries
- Vascular injury - uncommon, however the sequelae can be serious. Complete vascular assessment needs to be done on all patients with tibia fractures. Proximal tibial shaft fractures are at higher risk of causing a vascular injury
- Angular deformity - tibial varus angular deformity can occur in isolated tibial fractures. Therefore, close follow-up in the first 3 weeks is recommended
See fracture clinics for other potential complications.
References (ED setting)
Halsey MF, Finzel KC, Carrion WV, Haralabatos SS, et al. Toddler's fracture: presumptive diagnosis and treatment. J Pediat Ortho 2001; 21(2): 152-6.
Price CT, Flynn JM. Management of fractures. In Lovell and Winter's Pediatric Orthopaedics, 6th Ed, Vol 2. Morrissy RT, Weinstein SL (Eds). Lippincott, Philadelphia 2006. p.1430-521.
Mashru RP, Herman MJ, Pizzutillo PD. Tibial shaft fractures in children and adolescents. J Am Acad Ortho Surg 2005; 13(5): 345-52.
Henrich SD, Mooney JF. Fractures of the shaft of the tibia and fibula. In Rockwood and Wilkins' Fractures in Children, 7th Ed. Beaty JH, Kasser JR (Eds). Lippincott Williams & Wilkins, Philadelphia 2010. p.930-66.
Yang JP, Letts RM. Isolated fractures of the tibia with intact fibula in children: a review of 95 patients. J Pediat Ortho 1997; 17(3): 347-51.