Fracture Guideline Index
See also:
Neck of femur (NOF) fractures - Fracture clinics
- Summary
- How are they classified?
- How common are they and how do they occur?
- What do they look like - clinically?
- What radiological investigations should be ordered?
- What do they look like on x-ray?
- When is reduction (non-operative and operative) required?
- Do I need to refer to orthopaedics now?
- What is the usual ED management for this injury?
- What follow-up is required?
- What advice should I give to parents?
- What are the potential complications associated with this injury?
1. Summary
ED management
Neck of femur (NOF) fractures are uncommon in children but can have serious consequences. They are generally a result from higher energy trauma.
Prompt orthopedic treatment is required.
|
2. How are they classified?
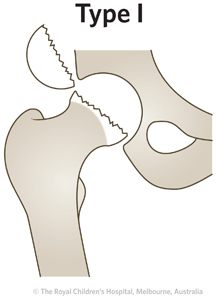
These fractures can be classified by the Delbet classification (Table 1).
Table 1: Delbet classification of neck of femur fractures.
Delbet type
|
Frequency
|
Description
|
|
5%
|
Fracture goes through the physis (transphyseal)
|
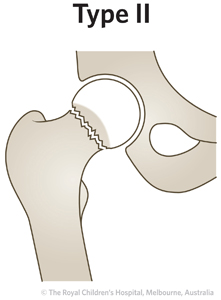
|
Most common
~50%
|
Fracture goes through the middle of the femoral neck (transcervical)
|
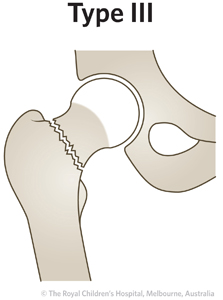
|
25-30%
|
Fracture goes through base of the femoral neck (cervicotrochanteric)
|
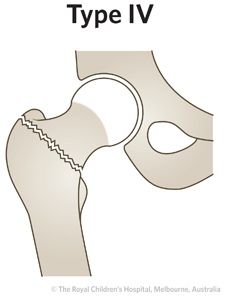
|
15%
|
Fracture goes between the greater and lesser trochanters (intertrochanteric)
|
3. How common are they and how do they occur?
These fractures are rare and account for less than 1% of all paediatric fractures. They generally occur from high energy injury mechanisms (such as a fall from a height or motor vehicle collision). Pathologic fractures can occur from lower energy injuries.
4. What do they look like - clinically?
The patient will have a painful leg or hip and will not want to weight bear. The leg may be shortened and externally rotated.
5. What radiological investigations should be ordered?
Anteroposterior (AP) pelvis and AP/lateral views of the affected femur should be obtained
6. What do they look like on x-ray?
Figure 1: Delbet type III femoral neck fracture.
7. When is reduction (non-surgical or surgical) required?
Reduction is required for all displaced fractures. This is performed in the operating theatre. All fractures need stabilisation. The method is dependent upon the patient age and fracture pattern.
8. Do I need to refer to orthopaedics now?
All NOF fractures require prompt orthopedic assessment.
9. What is the usual ED management for this injury?
Patients involved in high energy trauma, should be assessed by Advanced Trauma Life Support (ATLS) principles. Assessment should be made to identify the presence of any other injuries. Analgesia should be given. Prompt orthopedic consultation should be made.
10. What follow-up is required?
Any follow-up should be arranged by the orthopaedic service.
11. What advice should I give to parents?
The child will be admitted to the hospital for treatment of the injury by orthopaedics.
12. What are the potential complications associated with this injury?
- Avascular necrosis (AVN, also called osteonecrosis) of the femoral head - this is the most common complication following a NOF fracture. The risk of disruption of the blood supply to the femoral head is dependent on fracture type and age. The risk for a displaced Delbet type I fracture is up to 100%, for type II fracture is up to 61%, for type III fracture is up to 27% and for type IV fracture is 14%
- Coxa vara (neck shaft angle <120 degrees) - this is the second most common complication and has been reported to occur in up to 30% of cases. This can occur from progressive deformity in initially undisplaced fractures or from loss of reduction in displaced fractures. More severe coxa vara can cause abductor dysfunction and result in a Trendelenburg gait pattern
- Growth arrest - the physis of the femoral head contributes to approximately 15% of overall limb length (3-4 mm of growth per year). Reports of early physeal closure following NOF fractures vary in incidence of 5-65%. It is associated with AVN and transphyseal fixation. Premature physeal closure can result in coxa vara and limb length discrepancy
- Chondrolysis - this is uncommon but can be associated with osteonecrosis of the femoral head due to disruption of the blood supply to the cartilage of the femoral head
- Infection - this is uncommon after surgical fixation of femoral neck fractures. It is reported to occur in less than 1% of cases
See fracture clinics for other potential complications.
References (Emergency setting)
Boardman MJ, Herman MJ, Buck B, Pizzutillo PD. Hip Fractures in Children. J Am Acad Ortho Surg 2009; 17:162-73.
McCarthy JM, Noonan K. Fractures and traumatic dislocations of the hip in children. In Rockwood and Wilkins' Fractures in Children, 7th Ed. Beaty JH, Kasser JR (Eds). Lippincott Williams & Wilkins, Philadelphia 2010. p.769-96.