Fracture Guideline Index
See also:
Femoral shaft fracture - Fracture clinics
- Summary
- How are they classified?
- How common are they and how do they occur?
- What do they look like - clinically?
- What radiological investigations should be ordered?
- What do they look like on x-ray?
- When is reduction (non-operative and operative) required?
- Do I need to refer to orthopaedics now?
- What is the usual ED management for this injury?
- What follow-up is required?
- What advice should I give to parents?
- What are the potential complications associated with this injury?
1. Summary
All femoral shaft fractures should be assessed by the nearest orthopaedic on call service to evaluate the need for reduction and type of stabilisation.
Any patient with a significant mechanism of injury should be assessed via Advanced Trauma Life Support (ATLS) principles.
Femoral shaft fractures should be put into skin traction (10% of body weight) to help with pain management.
If the patient is to be transferred to another hospital, the leg should be immobilised in a Thomas type splint (if available) or a backslab.
Children that sustain femur fractures prior to walking age should be screened for non-accidental trauma.
|
2. How are they classified?
Femoral shaft (diaphyseal) fractures can be classified according to:
- Location - proximal, middle or distal third
- Amount of displacement, angulation and extent of shortening
- Fracture pattern - transverse, oblique, spiral or comminuted
3. How common are they and how do they occur?
Femoral shaft fractures represent approximately 1.6% of all pediatric fractures. It peaks in early childhood and early adolescence.
In older children, high energy trauma (e.g. motor vehicle accidents) is the mechanism of injury 90% of the time. In younger children, these fractures are usually due to falls. In children under four years of age, up to 30% of femur fractures are associated with non-accidental trauma. In children that are not yet walking, non-accidental trauma must be ruled out.
4. What do they look like - clinically?
The thigh will be swollen and deformed. Any movement through the leg will result in significant pain.
5. What radiological investigations should be ordered?
Anteroposterior (AP) and lateral x-rays of the femur should be ordered. The x-rays must show the full length of the femur (including hip and knee joint).
6. What do they look like on x-ray?

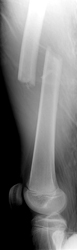
Figure 1: AP and lateral x-ray of the femur demonstrating a complete fracture of the femoral diaphysis.
7. When is reduction (non-operative and operative) required?
Femoral shaft fractures should be put into skin traction (~10% of body weight) to help with pain management. All femoral shaft fractures should be assessed by the nearest orthopaedic on call service to evaluate the need for reduction and type of stabilisation.
8. Do I need to refer to orthopaedics now?
All femoral shaft fractures should be referred for an urgent orthopaedic assessment in the ED.
Other indications for prompt consultation include:
- open fractures
- neurovascular injury with fracture
- polytrauma patient
9. What is the usual ED management for this injury?
Any patient with a significant mechanism of injury should be assessed via Advanced Trauma Life Support (ATLS) principles. Skin traction with approx 10% body weight should be applied. A femoral nerve block can be performed to help with pain management.
If the patient is to be transferred to another hospital, the leg should be immobilised in a Thomas type splint (if available) or a backslab.
Children that sustain femur fractures prior to walking age should be screened for non-accidental trauma.
Age, fracture pattern, fracture location, soft-tissue trauma and presence of associated injuries all influence the treatment modality (Table 1).
Table 1: Treatment options for femoral shaft fractures by age.
Age
|
Orthopaedic treatment options
|
≤ 6 months
|
Pavlik harness
Immediate spica cast
|
6 months to 5 years
|
Immediate spica cast
Traction → spica cast
|
5-11 years
|
Flexible intramedullary nailing
|
11 years - skeletal maturity
|
Rigid trochanteric entry nailing
Submuscular plating
Flexible intramedullary nail (only if <50 kg)
|
10. What follow-up is required?
Any follow-up should be arranged by the orthopaedic service.
11. What advice should I give to parents?
Outcomes for shaft fractures are generally good.
12. What are the potential complications associated with this injury?
- Leg length difference - femoral shaft fractures can overgrow up to 2 cm in the 2 years after the fracture. The fracture can also heal in a shortened position
- Malunion - the fracture is at risk of malunion, dependent on location and method of stabilisation
See fracture clinics for other potential complications.
References (ED setting)
Kocher MS, Sink EL, Blasier RD, Luhmann SJ, et al. Treatment of pediatric diaphyseal femur fractures. J Am Acad Ortho Surg 2009; 17(11): 718 -25.
Flynn JM, Skaggs DL. Femoral shaft fractures. In Rockwood and Wilkins' Fractures in Children, 7th Ed. Beaty JH, Kasser JR (Eds). Lippincott Williams & Wilkins, Philadelphia 2010. p.797 -841.