Fracture Guideline Index
See also: Distal tibia and or fibular physeal fracture
- Summary
- How are they classified?
- How common are they and how do they occur?
- What do they look like - clinically?
- What radiological investigations should be ordered?
- What do they look like on x-ray?
- When is reduction (non-operative and operative) required?
- Do I need to refer to orthopaedics now?
- What is the usual ED management for this injury?
- What follow-up is required?
- What advice should I give to parents?
- What are the potential complications associated with this injury?
1. Summary
Fracture type
|
ED management
|
Follow-up
|
Isolated undisplaced distal fibula physeal - Salter-Harris type I and II
|
Below-knee cast, non-weight bearing
|
Fracture clinic within 7-10 days with x-ray
|
Undisplaced distal tibia physeal
|
No reduction required. Immobilise in above-knee cast, non-weight bearing
For Salter-Harris type III and IV, discuss with orthopaedic on call service whether CT scan is required to confirm that fracture is truly undisplaced
|
Fracture clinic within 7 days with x-ray
|
Displaced distal tibia physeal
|
Closed reduction with above-knee cast, non-weight bearing.
If reduction not anatomic, discuss with orthopaedic on call service
For Salter-Harris type III and IV, refer to orthopaedic on call service
|
If treated with closed reduction, fracture clinic within 5 days
If treated operatively, to be arranged by orthopaedic service
|
Tillaux and triplane fracture <2 mm displacement
|
No reduction. Above-knee cast, non-weight bearing
Discuss with orthopaedic on call service whether CT scan is required to confirm that fracture is truly undisplaced
|
Fracture clinic within 7 days
|
Tillaux and triplane fracture >2 mm displacement
|
Refer to orthopaedic on call service. Typically requires operative management
|
To be arranged by orthopaedic service
|
2. How are they classified?
Distal tibial physeal fractures are classified by the Salter-Harris classification.
They can also be classified by the mechanism or direction of force applied to the injured ankle.
Due to the asymmetrical closure of the distal tibial physis (Figure 1) during early adolescence, transitional fractures can also occur.
- Tillaux fracture (Figure 2) - a Salter-Harris type III fracture involving avulsion of the anterolateral corner of the distal tibial epiphysis (the last portion of the physis to close)
- Triplane (Figure 3) - a Salter-Harris type IV fracture, which occurs in three planes (sagittal, transverse and coronal)
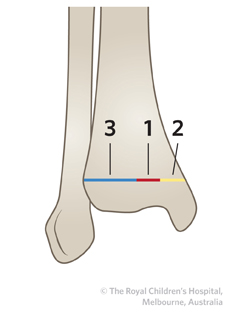
Figure 1: Closure of the distal tibial physis begins 1) centrally, followed by 2) medial closure and then 3) lateral closure.
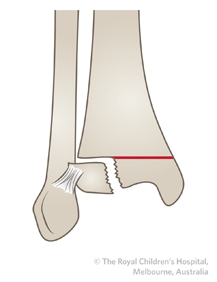
Figure 2: Tillaux fracture.
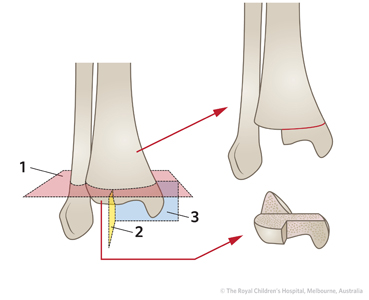
Figure 3: In a triplane fracture, the fracture line occurs in three planes. 1) Transverse (horizontal) plane - through the growth plate. 2) Coronal plane - through the posterior metaphysis. 3) Sagittal (anteroposterior; AP) plane - within the epiphysis and extending into the joint.
3. How frequent are they?
These injuries account for 25% of all physeal injuries. The distal tibia is the third most common physis to be injured.
4. How common are they and how do they occur?
These injuries commonly occur from a torsional or twisting mechanism about the ankle. The patient will present with a painful, swollen ankle. The foot can be in a deformed position. The patient will not want to weight bear.
!
|
Salter-Harris type I distal fibula fractures are the most common ankle fractures. They are often misdiagnosed as an ankle sprain or are missed. Tenderness will be located directly over the lateral malleolus rather than at the lateral ligaments
|
5. What radiological investigations should be ordered?
AP, lateral and mortise views of the ankle should be ordered.
If a tillaux or triplane fracture is suspected, discuss with orthopaedics for need to order a CT scan.
6. What do they look like on x-ray?
- Salter-Harris type I distal tibia fracture
In a Salter-Harris type I fracture, the fracture may not be evident on x-ray. The only radiographic finding may be soft tissue swelling over the distal fibular physis. It is usually diagnosed clinically with localised tenderness above the distal fibula.
- Salter-Harris type II distal tibia fracture

Figure 4: Displaced Salter-Harris type II distal tibia fracture with associated fibula fracture. This was initially managed with closed reduction. Due to poor alignment, a screw was inserted across the fracture site.
- Salter-Harris type III distal tibia fracture


Figure 5: Sixteen year old boy with a Salter-Harris type III fracture of the distal tibia. There is also a fracture of the distal shaft of the fibula.

A B
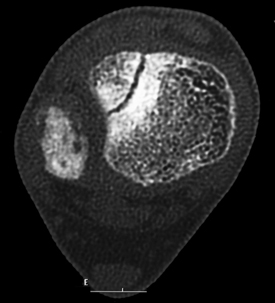
Figure 6: A) X-ray showing tillaux fracture (<2 mm). The fracture was treated non-operatively. B) Axial CT scan of the tillaux fracture, confirming that it is <2 mm displaced.

.jpg)
A B C
Figure 7: Ten year old female with triplane fracture. A) The AP view shows that the fracture is intra-articular. B) The oblique view shows opening of the lateral distal physis. C) The lateral view shows the opening of the physis anteriorly.
7. When is reduction (non-operative and operative) required?
All displaced or angulated fractures should have a reduction. Anatomic reduction is preferred. If less than anatomic, discuss with the orthopaedic service.
8. Do I need to refer to orthopaedics now?
Indications for prompt consultation include:
- open fractures
- Salter-Harris type III (including tillaux)
- Salter-Harris type IV (including triplane)
- neurovascular injury with fracture
- extreme swelling/compartment syndrome
- unable to achieve or maintain reduction (including if ED is not experienced in fracture reduction, splinting or casting)
9. What is the usual ED management for this injury?
Management depends on the location of the fracture, the degree of displacement, and the age of the child.
Fracture type
|
Type of reduction
|
Immobilisation method and duration
|
Isolated undisplaced distal fibula physeal - Salter-Harris type I and II
|
No reduction required
|
Below-knee cast, non-weight bearing
|
Undisplaced distal tibia physeal
|
No reduction required
For Salter-Harris type III and IV, discuss with orthopaedic on call service whether CT scan is required to confirm that fracture is truly undisplaced
|
Above-knee cast, non-weight bearing
|
Displaced distal tibia physeal
|
Closed reduction. If reduction is not anatomic, discuss with orthopaedic on call service
For Salter-Harris type III and IV, refer to orthopaedic on call service
|
Above-knee cast, non-weight bearing if managed with closed reduction.
|
Tillaux and triplane fracture <2 mm displacement
|
No reduction. Above-knee cast, non-weight bearing
Discuss with orthopaedic on call service whether CT scan is required to confirm that fracture is truly undisplaced
|
Above-knee cast, non-weight bearing
|
Tillaux and triplane fracture >2 mm displacement
|
Refer to orthopaedic on call service. Typically requires operative management
|
Refer to orthopaedic on call service. Typically requires operative management
|
10. What follow-up is required?
Isolated distal fibula physeal fractures should be followed up in fracture clinic in 7-10 days with repeat x-ray.
For undisplaced distal tibial physeal fractures, follow-up in fracture clinic should occur within 7 days with a repeat x-ray.
For displaced distal tibia physeal fractures managed with closed reduction and immobilisation should be reviewed in fracture clinic within 5 days.
For tillaux and triplane fractures < 2mm displacement, these can be followed up in 7 days.
11. What advice should I give to parents?
The child should remain non-weight bearing until instructed by orthopaedics.
There is a risk of compartment syndrome with the cast. Provide parents with "Caring for your child in a leg cast" and warning signs of a tight cast: increased pain despite analgesia, change in toes - colour, perfusion, increased swelling. Any concern should prompt immediate return to ED for evaluation.
The majority of fractures heal well and the outcome is excellent. With any fracture involving the growth plate, there is a risk of growth arrest. With any fracture involving the joint surface, there is a risk of future arthritis in that joint.
12. What are the potential complications associated with this injury?
- Growth arrest (one third of injuries)
- Compartment syndrome
- Arthritis
See fracture clinics for other potential complications.
References (ED setting)
Cummings RJ, Shea KG. Distal tibial and fibular fractures. In Rockwood and Wilkins' Fractures in Children, 7th Ed. Beaty JH, Kasser JR (Eds). Lippincott Williams & Wilkins, Philadelphia 2010. p.967-1016.
Schnetzler KA, Hoernschemeyer D. The pediatric triplane ankle fracture. J Am Acad Orthop Surg 2007; 15(12): 738-47.