Fracture Guideline Index
See also:
Olecranon fracture - Fracture clinics
-
Summary
-
How are they classified?
-
How common are they and how do they occur?
-
What do they look like - clinically?
-
What radiological investigations should be ordered?
-
What do they look like on x-ray?
-
When is reduction (non-operative and operative) required?
-
Do I need to refer to orthopaedics now?
-
What is the usual ED management for this fracture?
-
What follow-up is required?
-
What advice should I give to parents?
-
What are the potential complications associated with this injury?
1. Summary
|
!
|
The main complication of an olecranon fracture is failure to recognise an associated injury such as radial head dislocation.
|
|
Fracture type
|
ED management
|
Follow-up
|
|
Isolated undisplaced/stable fracture
|
Immobilisation in above-elbow backslab in 90 degrees elbow flexion with sling
|
Fracture clinic in 1 week with x-ray
|
|
Displaced/unstable and combined fracture
|
Place arm in above-elbow backslab in 90 degrees elbow flexion and refer to nearest orthopaedics on call service
Most require reduction/fixation
|
Follow-up to be arranged by orthopaedic service
|
2. How are they classified?
Olecranon fractures can be classified according to:
- Anatomical location: metaphyseal (most common), physeal (growth plate), epiphyseal
- Fracture pattern: transverse, oblique, longitudinal
- Displacement (whether undisplaced/stable or displaced/unstable)
- Associated injuries in elbow (e.g. radial head dislocation, lateral condyle fracture, radial neck fracture, supracondylar fracture)
3. How common are they and how do they occur?
These fractures account for 5% of all fractures of the elbow region. They are associated with other elbow injuries (e.g. radial head dislocation [Monteggia variant], lateral condyle fracture, radial neck fracture or supracondylar fracture). These usually occur as a result of direct trauma to the flexed elbow or indirect forces such as a fall on the outstretched hand, with a varus or valgus stress to the elbow joint.
4. What do they look like - clinically?
There is usually pain, tenderness and swelling at the fracture site, and decreased range of motion in the elbow.
Deformity is not typically a feature unless the olecranon fracture is associated with a radial head dislocation.
|
!
|
Always look for an associated injury, especially dislocation of the radial head.
|
5. What radiological investigations should be ordered?
An anteroposterior (AP) and lateral view of the elbow should be obtained. It important that the lateral view is a true lateral and that the AP clearly shows the relationship of the proximal radius and ulna to the humerus.
X-rays of the entire forearm are indicated if a radial head dislocation (Monteggia variant fracture) is suspected on the initial elbow films.
6. What do they look like on x-ray?
Isolated olecranon fracture


Figure 1: Isolated olecranon fracture (typically transverse and involve the elbow joint).
|
!
|
Always closely examine for other injuries around the elbow, e.g. radial head dislocations (Monteggia variant), radial neck fracture or lateral condyle fracture, etc.
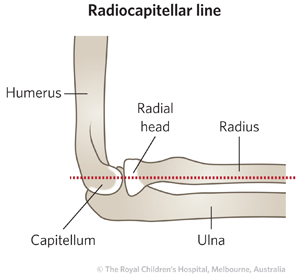
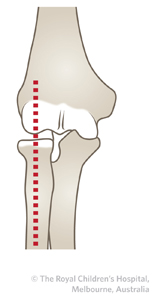
TIP:A line drawn down the shaft of the radius should point to the center of the capitellum in both AP and lateral x-ray views to exclude radial head dislocation.
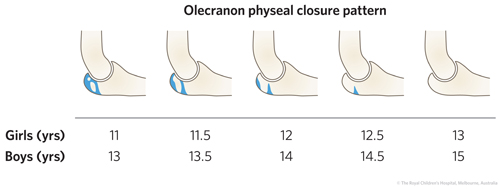
Beware mistaking the olecranon growth plate for a fracture and vice versa. If uncertainty exists then compare AP and lateral views of the contralateral elbow.
|
Olecranon fracture with associated injury
 |

|
|
Figure 2: Olecranon fracture associated with radial head subluxation dislocation (note lateral swelling).
|

|
|
Figure 3: Olecranon fracture with radial neck fracture.
|
7. When is reduction (non-operative and operative) required?
Approximately 80% of olecranon fractures are undisplaced or minimally displaced and require immobilisation only. All displaced fractures are unstable and will require reduction and fixation.
8. Do I need to refer to orthopaedics now?
Indications for prompt consultation include:
- Displaced fractures
- Open fractures
- Associated injuries around the elbow, e.g. radial head dislocation
Neurovascular injury with fracture (rare)
9. What is the usual ED management for this fracture?
Isolated undisplaced/stable fractures should be immobilised in an above-elbow backslab in 90 degrees elbow flexion.
For displaced and combined fractures, the arm should be placed in an above-elbow backslab in 90 degrees elbow flexion and referred to the nearest orthopaedic on call service. These fractures typically require operative management.
10. What follow-up is required?
Undisplaced/stable fractures should be seen in fracture clinic in one week, with x-ray at that visit.
For displaced fractures and those with associated injuries, follow-up care will be arranged by the orthopaedic service.
11. What advice should I give to parents?
A good outcome is expected for isolated stable/undisplaced fractures.
However, elbow injuries can be unpredictable and therefore close follow-up (including serial x-rays) is important. The outcome is not always good despite good management.
Joint stiffness may occur in olecranon fractures, with associated injuries, if there is a delay in recognition or if synostosis (Figure 4)/heterotopic ossification develops.

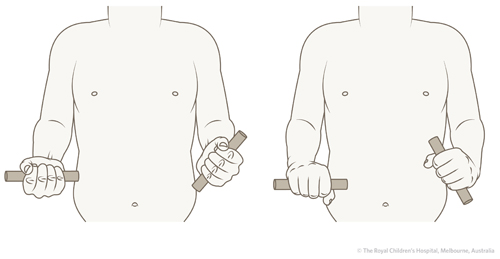
Figure 4: Synostosis of elbow showing limited supination and pronation of the left forearm.
12. What are the potential complications associated with this injury?
The main complication is failure to recognise an associated injury/joint instability upon initial presentation.
See
fracture clinics for other potential complications.
References (ED setting)
Evans MC, Graham HK. Olecranon fractures in children - Part 1: A clinical review; Part 2: A new classification and management algorithm. J Pediat Ortho 1999; 19(5): 559-69.
Green NE, Van Zeeland NL. Fractures and dislocations about the elbow. In Green N, Swiontkowski M. Skeletal Trauma in Children, 4th Ed. Saunders Elsevier, Philadelphia 2009. p.207-82.
Feedback
Content developed by Victorian Paediatric Orthopaedic Network.
To provide feedback, please email rch.orthopaedics@rch.org.au