Fracture Guideline Index
See also:
Galeazzi fracture-dislocation - Fracture clinics
-
Summary
-
How are they classified?
-
How common are they and how do they occur?
-
What do they look like - clinically?
-
What radiological investigations should be ordered?
-
What do they look like on x-ray?
-
When is reduction (non-operative and operative) required?
-
Do I need to refer to orthopaedics now?
-
What is the usual ED management for this fracture?
-
What follow-up is required?
-
What advice should I give to parents?
-
What are the potential complications associated with this injury?
1. Summary
Galeazzi fracture-dislocations are often missed and may be difficult to recognise. If there is an isolated radius fracture, always examine the distal radioulnar joint (DRUJ) on x-ray.
For all Galeazi fracture-dislocations, the arm should be splinted and the nearest orthopaedic on call service should be consulted.
2. How are they classified?
A Galeazzi fracture-dislocation is a fracture of the distal third of the shaft of the radius with a disruption to the DRUJ.
They can be classified by the direction of the ulna displacement:
|
Volar
|
Dorsal
|
3. How common are they and how do they occur?
These injuries are very rare in children. The most common mechanism is a fall on an outstretched hand with forearm rotation.
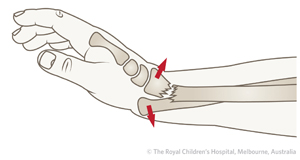
More common is the Galeazzi equivalent, where there is a distal radius fracture with a distal ulna physeal fracture but without disruption of the DRUJ (Figure 1).
Figure 1: A Galeazzi equivalent injury is characterised by fracture of the radius with fracture through the distal growth plate of the ulna but without disruption of the DRUJ.
4. What do they look like - clinically?
There will be swelling at the distal forearm and/or wrist. The forearm and wrist will be painful to move. Deformity through the forearm is usually clinically evident.
5. What radiological investigations should be ordered?
Anteroposterior (AP) and lateral x-ray of the forearm, which includes the wrist and elbow, should be obtained.
6. What do they look like on x-ray?
|
!
|
These fractures are often missed and may be difficult to recognise. If there is an isolated radius fracture, always examine the DRUJ on x-ray.
|
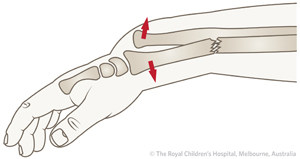
Figure 2: 14 year old boy with Galeazzi fracture-dislocation. The ulna is displaced dorsally.
7. When is reduction (non-operative and operative) required?
For children, most of these fractures can be managed with closed reduction. Fluoroscopy should be used to assess stability of the DRUJ after reduction.
Adolescents are more likely to need open or percutaneous fixation to stabilise the DRUJ after reduction.
8. Do I need to refer to orthopaedics now?
All Galeazzi fracture-dislocations should be referred to the nearest orthopaedic on call service.
Other indications for prompt consultation include:
- Open fractures
- Neurovascular injury with fracture
- Extreme swelling/compartment syndrome
9. What is the usual ED management for this fracture?
The arm should be splinted and the nearest orthopaedic on call service consulted.
10. What follow-up is required?
Follow-up in fracture clinic needs to be in 7 days with an x-ray. This should be arranged by the consulting orthopedic team after their reduction and stabilisation of the injury.
11. What advice should I give to parents?
The majority of these fractures will do well. Poor outcomes are usually a result of a delayed diagnosis or if the forearm has been immobilised in an incorrect position or in a below-elbow cast.
12. What are the potential complications associated with this injury?
Delayed diagnosis is a frequent complication. Nerve injury is uncommon, but cases have been reported with injuries to the ulnar nerve. This usually resolves with observation.
See
fracture clinics for other potential complications.
References (ED setting)
Atesok KI, Jupiter JB, Weiss AP. Galeazzi fracture. J Am Acad Ortho Surg 2011; 19: 623-33.
Rodríguez-Merchán EC. Pediatric fractures of the forearm. Clin Ortho Relat Res 2005; 432: 65-72.
Stutz C, Mencio G. Fractures of the distal radius and ulna: Metaphyseal and physeal injuries. J Pediat Ortho 2010; 30: S85-9.
Walsh HPJ, McLaren CAN, Owen R. Galeazzi fractures in children. J Bone Joint Surg 1987; 69(B): 730-3.
Waters PM, Bae DS. Fractures of the distal radius and ulna. In Rockwood and Wilkins' Fractures in Children, 7th Ed. Beaty JH, Kasser JR (Eds). Lippincott Williams & Wilkins, Philadelphia 2010. p.292-346.
Feedback
Content developed by Victorian Paediatric Orthopaedic Network.
To provide feedback, please email rch.orthopaedics@rch.org.au