See also:
Clavicle fractures - Fracture clinics
-
Summary
-
How are they classified?
-
How common are they and how do they occur?
-
What do they look like - clinically?
-
What radiological investigations should be ordered?
-
What do they look like on x-ray?
-
When is reduction (non operative and operative) required?
-
Do I need to refer to orthopaedics now?
-
What is the usual ED management for this fracture?
-
What follow-up is required?
-
What advice should I give to parents?
-
What are the potential complications associated with this injury?
-
Parent information fact sheet (PDF)
1. Summary
- Clavicle Fracture is a common injury in children, most often occurring after a simple fall onto an outstretched hand
- These most commonly occur in the middle third of the bone, with the vast majority healing well without intervention beyond sling immobilisation
- Follow-up must be planned for completely off-ended fractures in older children, and for lateral third fractures
- Medial third fractures are uncommon and require careful assessment for associated injuries, especially when displaced.
- All fractures should be assessed using the Advanced Trauma Life Support (ATLS) principles to ensure associated and potentially significant injuries are identified.
2. How are they classified?
Fractures of the clavicle can be classified by its anatomical location (Table 1):
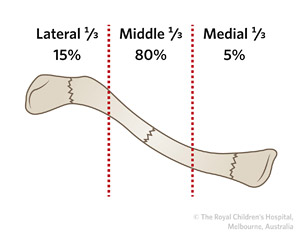
Table 1: Classification of clavicle fractures by location.
| Location |
Frequency |
Description |
|
Lateral third |
15% |
Around and lateral to coracoclavicular ligaments
Lateral ⅓ fractures are at higher risk of nonunion than other types |
|
Middle third or midshaft |
80% |
Defined by shortening/comminution/angulation |
|
Medial third |
5% |
- Bony injury alone
- Associated sternoclavicular dislocation
|
3. How common are they and how do they occur?
The clavicle is one of the most common fractured bones in children. Half of all paediatric clavicle fractures occur under the age of seven years. These heal quickly and recover fully.
Injuries are usually the result of a fall on an outstretched hand with the force transmitted up the arm.
A direct blow to the outer end of the clavicle (such as a fall onto the point of the shoulder during sporting activities or a striking injury) can be associated with distal third injuries and acromioclavicular joint disruption.
Clavicle fracture is also the most common perinatal fracture associated with birth trauma.
4. What do they look like - clinically?
The vast majority present with pain, swelling and deformity along the line of the clavicle, and a history of a fall onto an outstretched arm. Toddlers may present to ED with only history of avoiding use of the arm, as the trauma may not have been witnessed.
Fractures of the medial third are usually the result of high impact blunt force to the anterior chest (such as in a motor vehicle accident), and can be associated with neurovascular, pulmonary and cardiac (rare) injuries. Careful airway protection and neurovascular assessment is required.
!Careful neurological examination should be performed to define potential (but rare) associated brachial plexus injury.
Vascular assessment of the arm should also be performed as the subclavian artery runs closely apposed to the clavicle in the middle third.
5. What radiological investigations should be ordered?
Standard anteroposterior (AP) and AP with 15 degrees cephalic tilt x-ray of the clavicle will show the fracture in two planes and define displacement.
CT Scan is very seldom required. It may be needed in medial third injuries to assess tracheal impingement and thoracic anatomy, or in displaced lateral third injuries to assess the coraco-clavicular ligament, with orthopaedic consultation.
6. What do they look like on x-ray?
Middle third fracture

Seven year old boy with angulated (not translated) fracture of the middle third of the clavicle.
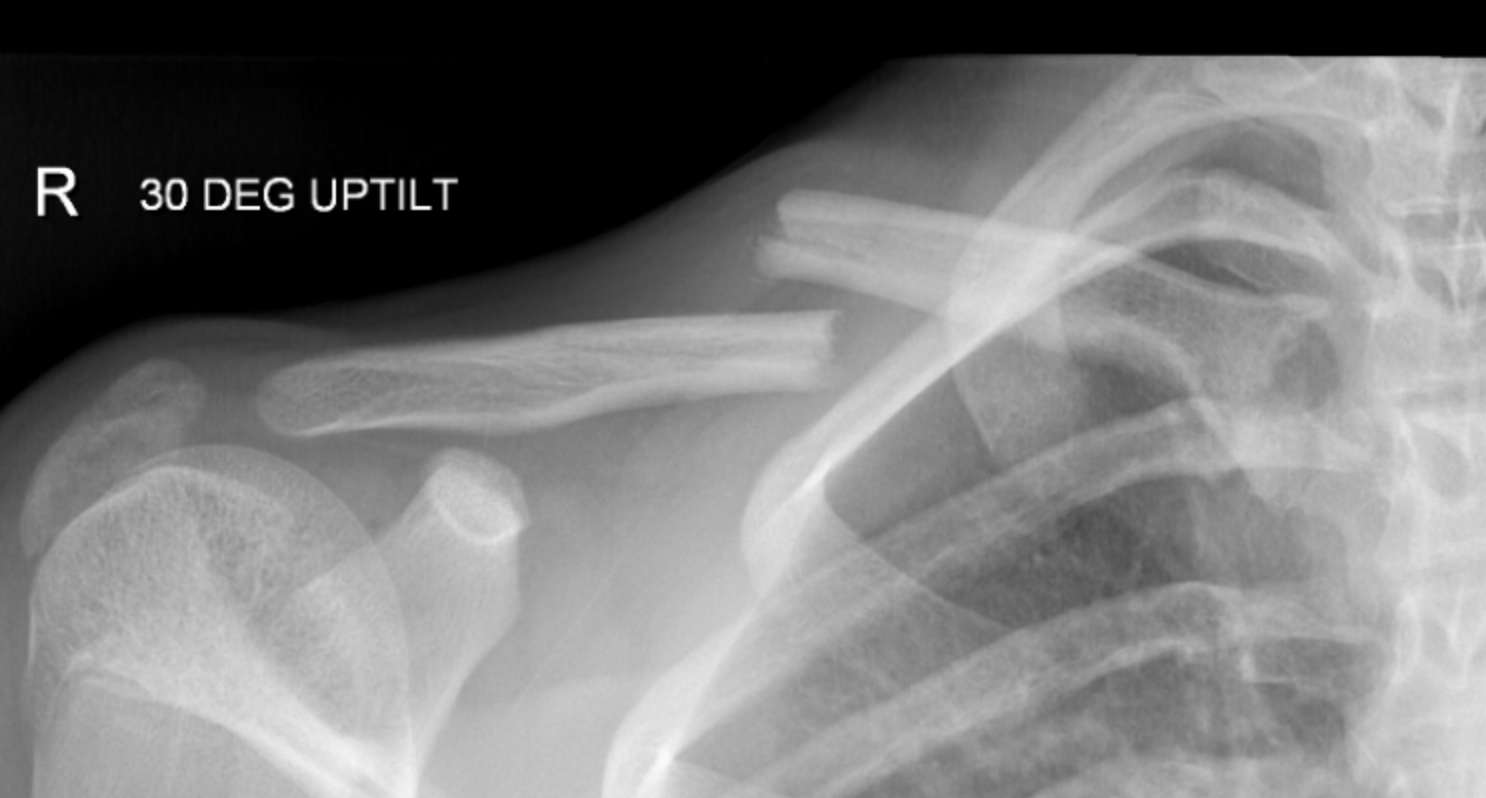
A middle third fracture with greater than 100% displacement
Lateral third

Figure 2: Undisplaced lateral third fracture of the clavicle in a 12 year old boy.
Sternoclavicular dislocation (posterior displaced)

A |
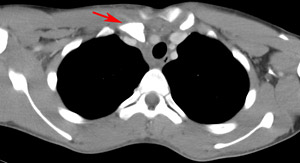
B |
Figure 3: A) 14 year old with posterior dislocation of the medial end of right clavicle. This is difficult to see on x-ray. B) The posterior dislocation (red arrow) is more evident on CT scan.
7. When is reduction (non operative and operative) required?
Reduction of middle-third clavicle fractures in ED is almost never required. Angulation is likely to improve with a supportive broad-arm sling, and later remodelling.
Indications for immediate orthopaedic referral are listed in point 8 below
Some older children with completely displaced & shortened fractures ultimately undergo open reduction following outpatient review, as in point 10 below.
8. Do I need to refer to orthopaedics now?
The majority of clavicle fractures are easily managed with a sling and analgesia.
Indications for immediate consultation include:
- Open fractures
- Displaced medial third fractures
- Neurovascular injury with fracture
- Skin integrity at risk over fracture
- Displaced lateral third fractures
- Pathological fractures
Orthopaedic consultation should also occur for middle third fractures in older children where there is
- Severe comminution or
- Complete displacement (off-ending), &/or
- Shortening >2cm
9. What is the usual ED management for this fracture?
|
Fracture type |
Type of reduction |
Immobilisation method & duration |
|
Middle third |
Generally no reduction required |
Broad arm sling to support limb for 2-3 weeks or until comfortable
Regular analgesia as required |
|
Lateral third |
If undisplaced, no reduction required
If displaced, refer to the nearest orthopaedic service on call |
Broad arm sling to support limb for 4 weeks or until comfortable
Regular analgesia as required |
|
Medial third |
If undisplaced, no reduction required
If displaced, immediate referral to the nearest orthopaedic service on call |
Broad arm sling to support limb |
10. What follow-up is required?
Middle third fracture
Children
<11 years old with undisplaced fractures do not usually require follow-up by a GP or fracture clinic. Repeat x-rays are usually not required, as the remodelling capacity in this age group is very high. Mobilisation out of the sling commences at two weeks depending on pain control, with contact sports delayed until 6 weeks.
GP review of at 1-2 weeks post injury will consist of familiarisation with the history and radiographs and assessment of pain and function. Any persistent pain/tenderness at the fracture site not improving at 2-4 weeks may be an early indicator of non-union, and should prompt repeat X-rays and orthopaedic referral.
All children >14 years with completely displaced fractures (i.e. off-ended) should be referred to an orthopaedic fracture clinic with repeat radiograph, as this cohort is at the highest risk for non-union.
Other children ≥11 years old, or displaced fractures
<11 years old, can be followed up with the family GP in approximately one week. Persistent pain not improving at the fracture site at 2-3 weeks, with ongoing disability may be an early indicator for non-union, and should prompt repeat xrays and orthopaedic referral.
Lateral third fracture and medial fractures/dislocations
Follow up in orthopaedic fracture clinic
Neonatal clavicle fractures
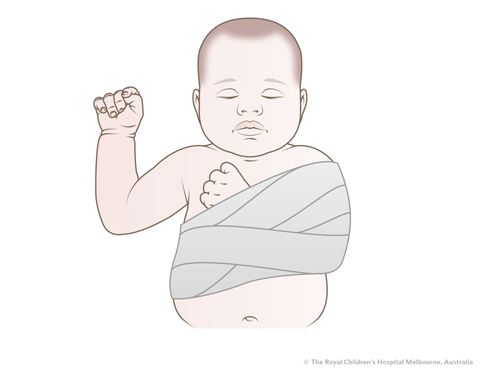
Simple Swathe as shown for 2 weeks
11. What advice should I give to parents?
The majority of uncomplicated middle third fractures will have excellent functional and cosmetic outcomes.
Provide parent with
fracture of the clavicle (collarbone) fact sheet.
Pain from the fracture and restriction of movement are usual for 2-3 weeks and will require regular analgesia.
The child should re-attend if pain is increasing. Contact sports and activities should be avoided for approximately six weeks post removal of sling. A lump usually develops at the fracture site, which may be visible and palpable for at least one year and then resolves.
12. What are the potential complications associated with this injury?
- Neurovascular complications are rare
- Nonunion is uncommon, but is more likely in the older adolescent or in lateral third fractures
- Malunion - palpable or visual lump, which diminishes with remodelling
- Degenerative arthritis if acromioclavicular joint intra-articular incongruence
See
fracture clinics for other potential complications.
References (ED setting)
Asadollahi, S. and Saremi, S. Surgical management of displaced midshaft clavicle fracture in the skeletally immature patient - What is the Hunter JB. Fractures around the shoulder and humerus. In Children's Orthopaedics and Fractures,3rd Ed. Benson M, Fixsen J, Macnicol M, Parsch K (Eds). Springer, London 2010. p.717-30.
Lenza M, Belloti JC, Andriolo RB, Gomes Dos Santos JB, Faloppa F. Conservative interventions for treating middle third clavicle fractures in adolescents and adults. Cochrane Database Syst Rev 2009; CD007121.
Mehlman C. et al. Operative treatment of completely displaced clavicle shaft fractures in children, J Pediatr Orthop 2009; 29(8):851-5
Klein SM, Badman BL, Keating CJ, Devinney DS, Frankle MA, Mighell MA. Results of surgical treatment for unstable distal clavicular fractures. J Shoulder Elbow Surg 2010; 19: 1049-55.
Pecci M. & Kreher, J. Clavicle Fractures Am Fam Physician. 2008 Jan 1;77(1):65-70.
Simon RR, Sherman SC, Koenigsknecht SJ. Clavicle fractures. In Emergency Orthopaedics - The Extremities. 5th Ed. McGraw-Hill, Chicago 2007. P.285-7.
Vargas-Vila, M et al. The Community Orthopaedic Surgeon Taking Trauma Call: Pediatric Midshaft Clavicle Fracture Pearls and Pitfalls, J Orthop Trauma 2019;33:S1-S5
Young SJ, Barnett PL, Oakley EA. Fractures and minor head injuries: Minor injuries in children II. Med J Aust 2005; 182: 644-8.