See also
Urinary Tract Infection
Febrile Child
Acute pain management
Key points
- Suprapubic aspirate is the gold standard for obtaining urine specimens for culture in children under 2 years
- Suprapubic aspirate is a simple, safe, rapid and effective procedure
- The use of ultrasound increases the success of the procedure
- Any growth of pathogenic bacteria in an SPA specimen is felt to be significant
Background
Indications:
- Young unwell infants for whom there is a need to obtain specimens as part of a septic work-up where antibiotic administration should not be delayed while awaiting a clean-catch urine
- For a child (<2 years) when it is deemed important to confirm a UTI. eg in a child with recurrent urinary tract infections with positive cultures but minimal cellular response
- Children with previous UTIs with unusual or resistant organisms
- Children on prophylactic antibiotics
Contraindications:
- Bleeding diathesis
- Abdominal distension
- Massive organomegaly
- Urogenital or gastrointestinal abnormality
- Overlying soft tissue infection
Potential
Complications:
Microscopic haematuria is common. There are some rare complications which include: macroscopic haematuria, bladder haematoma, bladder haemorrhage, intestinal perforation.
Equipment
- One assistant to hold the infant (not parent)
- Specimen jar for urine
- 23G needle (25G for premature infants)
- 3 mL or 5 mL syringe
- Sterile gloves
- Ultrasound/Bladder scanner and gel if available
Analgesia, Anesthesia, Sedation
- Topical anaesthetic cream should ideally be used except where specimens are required urgently (eg prior to starting antibiotic treatment in a septic infant).
- Oral sucrose should be used for infants
<3 months (see Acute pain management).
Procedure – step by step
- Never undo the nappy until you have
a urine jar handy and someone ready to catch!
- The patient should not have passed urine for 30 minutes prior to procedure
- Verbal consent is adequate
- Do the SPA before collecting blood or CSF unless the patient has voided recently.
- 'Blind' SPA has an approximately 50% chance of obtaining urine. The use of ultrasound increases the chance of success to 80-90%. Ultrasound is a useful tool to determine when NOT to do an SPA. There are two types of ultrasound that can be utilized:
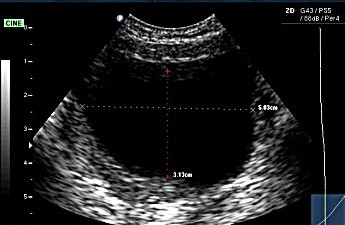
- Real time 2D ultrasound provides visualisation of the bladder and an estimation of its fullness. It is more accurate than the automated bladder ultrasound and should be used in preference to this if expertise in using a 2D ultrasound is available.
- Automated bladder ultrasound provides a urine volume in mL. It does not visualise the bladder. Its ability to detect volumes less than 20 mL is poor. It should be used only when 2D ultrasound equipment or expertise is not available.
- To minimise likelihood of voiding it is helpful to use warmed gel which should be placed on the ultrasound probe and not directly on the skin.
Real time ultrasound images:
| Full bladder |
|
| Transverse image |
Longitudinal image |
 |
.2.jpg) |
| |
|
| Empty bladder |
|
| Transverse image |
Longitudinal image |
 |
 |
Flow chart for use of ultrasound
.png)
What to do if a bladder ultrasound is not available
Factors increasing the likelihood of a successful SPA:
- History of no voiding in the past 30 minutes, and the presence of a dry nappy
- Pre-hydration
- Bladder dull to percussion
Flow Chart if no ultrasound or bladder scanner available
.png)
SPA Method
-
Assistant to hold the infant supine with legs extended and together (see picture below). To prevent voiding in boys, the shaft of the penis should be squeezed to occlude the urethra
- Identify insertion point: midline, lower abdominal crease. See
SPA Procedure - Identifying insertion point
- Standard aseptic non-touch technique with sterile gloves is preferred
- Wipe the overlying skin with an alcohol swab
- Insert needle perpendicular to the skin in all directions. Do not aim the tip of the needle down into the pelvic region. (The bladder in a baby is predominantly an abdominal rather than pelvic organ). The skin should be punctured quickly as if popping a balloon with a needle.
Insert needle to the hub and aspirate. If urine is not immediately aspirated, continue aspirating as the needle is withdrawn
- If unsuccessful, withdraw the needle to just under the skin, and advance at an angle with the needle aimed further away from the pelvis. Do not repeat this procedure more than once
- If urine is obtained, remove needle and place urine into sterile urine jar
 Positioning of infant during the procedure
Positioning of infant during the procedure
Post-Procedure Care
No specific care required.
Alternatives
if procedure not successful
- If SPA cannot be obtained a catheter sample should be collected (see flow chart above)
- If urine is unable to be collected in an unwell child, do not delay treatment (eg antibiotics)
- A sample of urine should still be collected as soon as possible for a microscopy
Consider consultation with local paediatric
team when
- The child is febrile and less than 3 months of age
- The child appears unwell and/or may require escalation of care outside of the immediate health care setting
Consider transfer when
Child requiring care above the level of comfort of the local hospital
For emergency advice and paediatric or neonatal ICU transfers, call the Paediatric Infant Perinatal Emergency Retrieval (PIPER) Service: 1300 137 650.
Parent information sheet
Kids Health Info
Urine Samples
Last updated January 2019