See also:
SSRI Poisoning
SNRI Poisoning
Poisoning – Acute Guidelines for Initial Management
Resuscitation
Key points
- Be aware of the possibility of serotonin toxicity diagnosis when patients have been exposed to any of the agents implicated
- Serotonin toxicity encompasses a wide spectrum of clinical signs and symptoms
- Severe serotonin toxicity is a medical emergency. Untreated, serotonin toxicity can progress to multi-organ failure and death. Severe cases should be managed in a Paediatric ICU
For 24 hour advice, contact the Poisons Information Centre 13 11 26
Background
The term Serotonin Syndrome has been replaced by Serotonin Toxicity to reflect the varied presentation and severity of serotonin poisoning rather than a single clinical entity (syndrome)
- Serotonin toxicity is the clinical manifestation of excessive central and peripheral serotonergic neurotransmission
- It manifests as a wide variety of signs reflecting the triad of CNS, autonomic and neuromuscular dysfunction
- There is a spectrum of severity ranging from mild symptoms to a severe life-threating condition
If serotonin toxicity is suspected please seek senior advice and discuss with toxicologist
Serotonin toxicity can occur in the following clinical settings:
- Drug interaction between two serotonergic agents (most common)
- On introduction or increase in dose of a single serotonergic drug
- Change in therapy from one serotonergic drug to another without adequate washout period
- Interaction between a serotonergic agent and an illicit drug or herbal preparation
- Deliberate self-poisoning with serotonergic agents
- Accidental ingestion of serotonergic agents
Risk assessment
Patients requiring assessment
- Any symptomatic patients
- All patients with deliberate self-poisoning or significant accidental ingestion of serotonergic agents
Patients who have co-ingested a number of serotonergic agents are at significantly greater risk of serotonin toxicity
|
Agents Commonly Implicated in the Development of Serotonin Toxicity
|
|
Class
|
Drugs
|
|
Antidepressants
|
Monoamine oxidase inhibitors (MAOIs)
Tricyclic antidepressants (TCAs)
Selective serotonin re-uptake inhibitors (SSRIs)
Serotonin and noradrenaline re-uptake inhibitors (SNRIs)
Lithium
Bupropion
|
|
Analgesics and antitussives
* High risk
|
Tramadol*
Pethidine*
Dextromethorphan*
Methadone
Tapentadol
Fentanyl
|
|
Drugs of abuse
|
MDMA (ecstasy)
LSD
Amphetamines
Cocaine
|
|
Antiemetics
|
Ondansetron
Granisetron
Metoclopramide |
|
5-HT1 agonists
|
Sumatriptan
|
|
Herbs
|
St John's Wort
Ginseng
Nutmeg
|
History and Physical Examination
Diagnosis of serotonin toxicity is based on:
- A history of ingestion of one or more serotonergic agents
- Clarify the drugs recently prescribed and if any illicit drugs or herbal preparations ingested
- Ascertain the amounts ingested and when the ingestion occurred
- The presence of characteristic symptoms and physical signs (see table)
|
Serotonin Toxicity
|
|
Mild
|
Moderate
|
Severe
|
|
Inducible clonus
Tachycardia
Tremor
Anxiety
Lower limb hyper-reflexia
|
Agitation
Sustained clonus
Ocular clonus
Hyperthermia
<39oC
|
Hyperthermia >39oC
Seizures
Muscle rigidity
Severe agitation, confusion
|
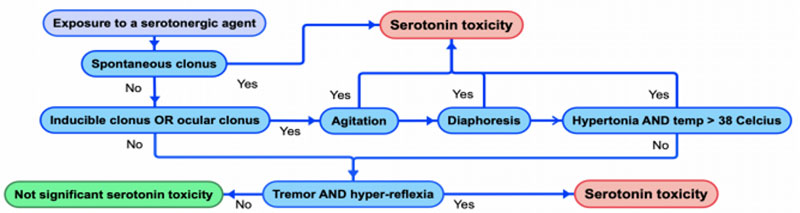
Hunter Serotonin Toxicity Criteria
Reference: Austin Clinical Toxicology Service Guidelines: Serotonin (5HT) toxicity
Differential Diagnosis
Serotonin toxicity may mimic other serious conditions which should be considered and excluded such as:
- Neuroleptic malignant syndrome
- Withdrawal syndromes
- Malignant hyperthermia
- CNS infection
Always check for Medicalert bracelet in any unconscious patient, or any other signs of underlying medical condition (fingerprick marks etc)
Management
Investigations
- 12 lead ECG, blood glucose and paracetamol concentration in deliberate self-poisoning
- Depending on severity further investigations may be necessary to exclude significant complications including urea, creatinine, electrolytes, creatinine kinase, troponin
- Depending on the drug/agent ingested further investigations may be needed (Discuss with toxicologist)
Treatment
Cease any causative agents
Supportive care and monitoring of temperature, muscle tone and mental status
Serotonin toxicity can be treated with titrated intravenous benzodiazepines in discussion with toxicologist
If symptoms are refractory a serotonin antagonist such as cyproheptadine or chlorpromazine may be considered in discussion with a toxicologist
Cyproheptadine
Oral
<7 years: 2 mg
≥7 years: 4 mg
If continuing treatment for prolonged symptoms use the same dose 3 times a day until symptoms are resolved - usually within 24 hours
Chlorpromazine
Intravenous
Chlorpromazine 0.5 mg/kg (max 25 mg) in sodium chloride 0.9% 10 mL/kg (max 500 mL) IV, over 30 to 60 minutes.
Repeat the dose every 6 to 8 hours until symptoms resolve, provided the patient is not hypotensive
Depending on the drug/agent ingested further treatment may be needed, discuss with toxicologist
Standard procedures and supportive care
Consider consultation with local paediatric team when
- Child is symptomatic: requires admission for monitoring and treatment if necessary
- Children at risk of serotonin toxicity with deliberate self-poisoning or significant accidental ingestion should be observed for symptoms for a minimum of 12 hours
- Any child or adolescent presenting with intentional overdose as admission should be considered
Consult Victorian Poisons Information Centre 13 11 26 for advice
Consider transfer when
- Children require care beyond the comfort level of the current hospital
- Patients who develop severe serotonin toxicity should be managed in PICU
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services.
Consider discharge when
Normal GCS
Normal ECG
Period of observation as above
- Resolution of symptoms with complete recovery can be expected in 24-48 hours
Assessing risk and connecting to community services
- Prior to discharge, adolescents who present with deliberate ingestions need a risk assessment regarding the likelihood of further ingestions or other attempts to self-harm
- Assessment of other drug and alcohol use should also be undertaken
- If, after risk assessment, it is deemed safe to discharge the child or adolescent from hospital, but ongoing mental health or drug and alcohol needs are identified, they should be linked with appropriate services (see links below for services in the State of Victoria)
Discharge information and follow-up:
Parent Information Sheet:
Poisoning prevention for children
Poisons Information Centre: phone 13 11 26
Victoria
Last Updated July 2021