See also
Abdominal pain – acute
Acute pain management
Key points
- The diagnosis of intussusception requires a high index of suspicion. Consider intussusception in infants and children with intermittent distress, vomiting or isolated unexplained lethargy
- Delayed presentation of intussusception can manifest as small bowel obstruction, bowel perforation, peritonitis and/or shock
- Ultrasound is the initial study of choice
Background
Intussusception is the invagination (telescoping) of a proximal segment of bowel into the distal bowel lumen. The commonest site is a segment of ileum moving into the colon through the ileo-caecal valve. This process leads to bowel obstruction, venous
congestion and bowel wall ischaemia. Perforation can occur and lead to peritonitis and shock
- The triad of intermittent abdominal pain, palpable abdominal mass and red currant jelly stools occurs in only 1/3 of children
- May occur at any age, but most commonly between 2 months and 2 years of age
- Most cases are idiopathic (90%)
- In older children, a pathological lead point may be the cause
Assessment
History
- Intermittent
pain or distress
- Episodes can recur within minutes to hours and may increase in frequency over the next 12–24 hours
- The child may appear very well between episodes
- Pallor, especially during episodes
- Lethargy may be the only presenting symptom. It may be profound, episodic or persistent
- Vomiting is usually a prominent feature (but bile stained
vomiting is a late sign and indicates a bowel obstruction)
- Diarrhoea is quite common initially and can lead to a misdiagnosis of gastroenteritis. Rectal
bleeding or the classic “red currant
jelly” stool are late signs suggesting bowel ischemia and infarction
Additional risk factors
- Recent intussusception (may present with more subtle symptoms)
- Potential lead point – eg Meckel’s diverticulum, Henoch Schonlein Purpura, lymphoma, luminal polyps (eg Peutz Jegher Syndrome)
- Recent bowel surgery
- Recent rotavirus vaccination
Examination
- Abdominal mass may be felt – typically a sausage shaped mass in the right abdomen, crossing the midline in the epigastrium or behind umbilicus (in 2/3 of children). The abdominal mass may be subtle and examination is best performed when the child is
settled in between episodes
- Abdominal distension suggests bowel obstruction
- Tenderness or guarding may suggest perforation and peritonitis
- Inspection of the nappy and perianal region should be done. A rectal examination is rarely indicated
- Infants may present with Hypovolaemic shock
Management
- Analgesia and resuscitation should precede investigation (see flowchart below)
- Secure IV access for all children suspected to have intussusception before diagnostic imaging
- Treat hypovolaemic shock with IV boluses of 20 mL/kg normal saline
- Give adequate analgesia (usually intranasal fentanyl or IV morphine). See Acute pain management
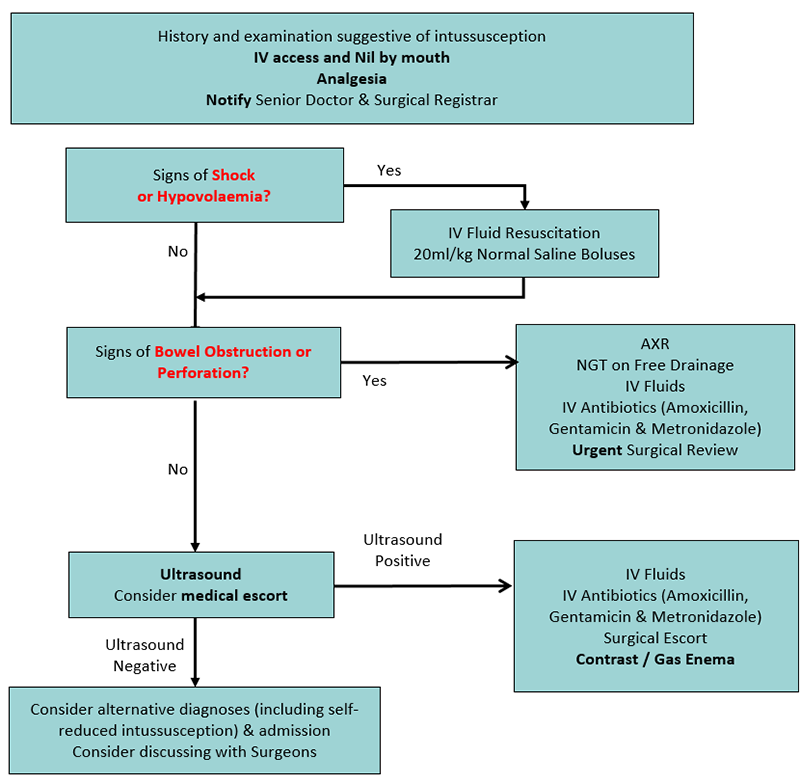
- Involve the surgical team early
- Keep nil orally
- Pass nasogastric tube if bowel obstruction or perforation on AXR, or if planning transfer by air
- Children with intussusception can decompensate while undergoing ultrasound and/or air enema. Ensure medical or nursing escorts are capable of providing resuscitation if needed
Investigations
Ultrasound scan
- High sensitivity (>98%) and specificity (>98%) when performed by an experienced paediatric ultrasonographer
- Point of Care Ultrasound can be used to confirm the diagnosis of intussusception by appropriately trained clinicians. It should not be used to exclude the diagnosis
Abdominal
X-Ray
- Perform AXR only if there are signs of obstruction or perforation
- A normal AXR does not exclude intussusception (sensitivity
<50%)
- Signs suggesting intussusception on an abdominal x-ray include:
- an abnormal gas pattern, with an empty right lower quadrant and visible soft tissue mass in the upper abdomen
- a soft tissue mass surrounded by a crescent lucency of bowel gas (crescent sign)
- lack of faecal material in the large bowel
- signs of small bowel
obstruction
- pneumoperitoneum indicating bowel perforation
Contrast / gas enema
- The enema may be used diagnostically and therapeutically in consultation with a surgical team
- There is a small risk of bowel perforation and bacteraemia during the gas enema. Therefore, the enema is performed where paediatric surgery is available in case of the need for laparotomy. Usually, a surgical doctor, as well as a suitably trained nurse, will
accompany the child with appropriate resuscitation equipment
- Contraindicated if peritonitis, shock, perforation, or an unstable clinical condition is present
Blood tests
- Blood glucose
- Venous Gas, FBE and UEC if the child looks unwell
- Blood group and hold prior to theatre
Consider consultation with local paediatric team when
There is suspicion of intussusception – (all suspected cases)
Consider transfer when
Child requiring care beyond the capability of the hospital
Note: when transferring infants or children with possible surgical conditions, ensure they have adequate analgesia, venous access and intravenous fluids prior to transfer, as third space losses can be large and lead to haemodynamic collapse. Consider a nasogastric tube on free drainage if
transferring by air.
For emergency advice
and paediatric or neonatal ICU transfers, see Retrieval Services
Parent information
Abdominal pain
Reducing your child’s pain during investigations and procedures
Pain relief for children
Intussusception
Last Updated August 2019