See also
Resuscitation: Care of the seriously unwell child
Resuscitation: Hospital management of cardiopulmonary arrest
Intravenous fluids
Electrolyte
abnormalities
Background
- Hyperkalaemia: serum K+ >5.5 mEq/L, (N range = 3.5-5.0 mEq/L), or >6.0 mEq/L in neonates
- Hyperkalaemia is potentially life threatening, and can result in cardiac arrhythmias and sudden death
Causes:
- Hyperkalaemia as an artefact of collection process or technique
- Decreased excretion (frequent cause)
- Renal diseases: Acute/chronic renal failure, renal anomaly
- Adrenal mineralocorticoid deficiency
- Transcellular shift
- Acidosis eg Diabetic ketoacidosis, lactic acidosis
- Increased production (Most often if in association with renal dysfunction)
- Extensive trauma, rhabdomyolysis (crush injury, convulsion, infection), haemolysis, tumour lysis syndrome, burns
- Exogenous source
- Iatrogenic potassium administration (oral, IV)
- Increased ingestion
- Massive transfusion
- Medication
- eg NSAID, trimethoprim, heparin, chemotherapy, K-sparing diuretic, ACE inhibitor, beta blockers, succinylcholine, digoxin, mannitol
Assessment
History and examination:
- Look for possible causes (see above)
- Hyperkalaemia can be initially asymptomatic or can presents with severe symptoms/signs:
- Respiratory depression
- Palpitations, arrhythmia, cardiac arrest
- Paraesthesia, flaccid paralysis
- Ileus
- Confirm that potassium in IV fluids and oral potassium supplements are stopped
- Assess the patient's medication list - stop drugs that increase potassium or reduce its excretion
Investigation and monitoring:
Note: Patients with moderate or severe hyperkalaemia need continuous cardiac monitoring and IV access
- Level of potassium should be confirmed with a second sample
- If patient has renal dysfunction (renal failure or other renal disease), assume potassium level correct until proven otherwise
- Acute increase of potassium is associated with higher risk of arrhythmia
- Do an ECG to identify conduction disturbance:
- Peaked T wave (early)
- Prolonged PR, flattening of P wave, widening of QRS (increased risk of arrhythmia)
- Absence of P wave, sine wave (fusion of QRS and T wave)
- Ventricular arrhythmia, asystole
Note: A normal ECG does not exclude risk for arrhythmia, as life threatening arrhythmia can occur without warning
- Complete investigations and consider causes of hyperkalaemia:
- Urea, creatinine and electrolytes
- Glucose
- Venous blood gas
- +/- Urine analysis and urinary electrolytes
- Consider other investigations depending on cause:
- CK
- Cortisol, aldosterone and hormonal precursor levels (particularly if hyponatraemic)
- Level of digoxin (if relevant)
Treatment
If pulseless arrhythmia, see Resuscitation
***Stop any source of potassium intake - IV fluid, parenteral alimentation, dietary supplement (including NGT feeding) and any potassium-sparing medication
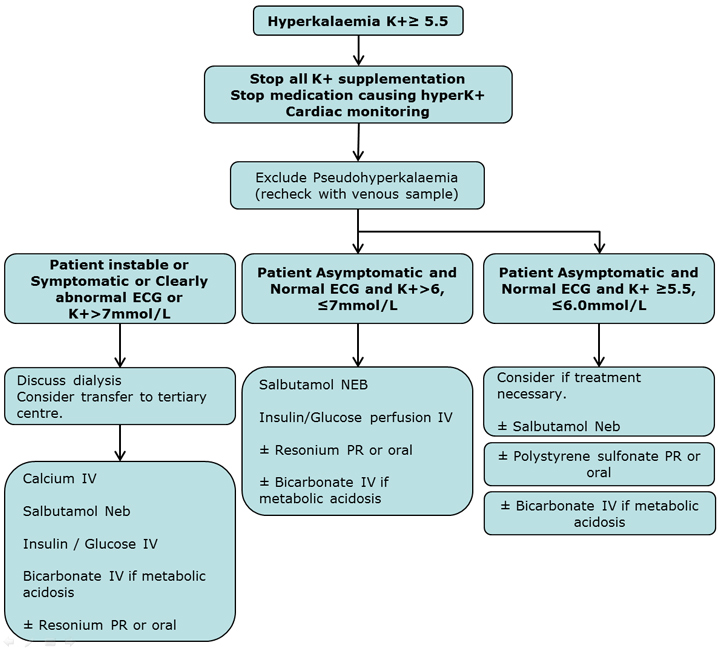
Severe hyperkalaemia
- K+ >7.0 mEq/L or at risk of increasing and/or
- Patient symptomatic and/or
- ECG disturbance:
- Calcium IV
- Salbutamol neb
- Insulin/glucose IV
- Bicarbonate IV if metabolic acidosis
- Dialysis:
- Urgent if unstable
- Rapid if stable but symptomatic or abnormal ECG
- Consider if asymptomatic but severe hyperkalaemia
- Resonium (Polystyrene sulfonate) PR (if dialysis unavailable)
Consider hydrocortisone 1-2 mg/kg IV if suspicion of adrenal insufficiency
Moderate hyperkalaemia
- K+ 6-7
- Patient asymptomatic
- Normal ECG
- Salbutamol neb
- Insulin/glucose IV
- Resonium (Polystyrene sulfonate) PR or oral
- Bicarbonate IV if metabolic acidosis
Mild hyperkalaemia
- K+ >5.5
- Patient asymptomatic
- Normal ECG
- Consider no treatment
- Stop K supplements
- Recheck result
- Salbutamol neb
- Polystyrene sulfonate PR or oral (resonium)
- Bicarbonate IV if metabolic acidosis
Therapies:
Calcium:
2 solutions :
- Calcium gluconate 10%: 0.5 mL/kg slow IV injection
- 2-5 minutes if unstable, over 15-20 min if stable (Max: 20 mL)
- Preferable if only peripheral line available
OR
- Calcium Chloride 10% : 0.1-0.2 mL/kg slow IV injection (as above) (Max: 10 mL)
Note: Give under cardiac monitoring, discontinue if HR dropping significantly
Avoid extravasations
NOT to be given simultaneously with bicarbonate
NOT to be given if digoxin toxicity
Onset of Action:
<3 minutes, should see normalisation of ECG. If not: repeat dose (twice)
Duration: ~30 minutes
Salbutamol:
- Salbutamol: nebulisation
- Less than 25 kg : 2.5 mg neb 1-2 hourly
- More than 25 kg : 5 mg neb (Adu max 10-20 mg) 1-2 hourly
- Salbutamol : IV *Only if severe hyperkalaemia after discussion with senior doctor from tertiary centre with monitoring for tachycardia
Onset of Action: 30 minutes
Duration: 2-3 hours
Insulin/glucose
to be given at the same time
If severe hyperkalaemia:
- Dextrose 10% : 5 mL/kg IV bolus (if no hyponatraemia)
- Insulin short action: 0.1 U/kg IV bolus (max 10 units)
Then followed by infusion insulin/glucose (see below)
If moderate hyperkalaemia:
- Dextrose 10% IV at maintenance with 0.9% sodium chloride (normal saline)
- Insulin short action infusion : 0.1 U/kg/h IV
Note: Close monitoring of glucose every 30-60 minutes
Onset of Action: 15 minutes
Duration: peak 60 minutes, 2-3 hours
Bicarbonate
In metabolic acidosis only
Severe
hyperkalamia and metabolic acidosis
- Sodium Bicarbonate 8.4% 1 mmol/mL : 1-3ml/kg IV over 5 minutes
Mild to moderate
hyperkalaemia and metabolic acidosis:
- Sodium Bicarbonate 8.4% 1 mmol/mL : 1 mL/kg slow IV infusion over 30 minutes
Note: Do NOT give simultaneously with Calcium
Onset of Action: 30-60 minutes
Duration: 2-3 hours
Dialysis
To be organised with local paediatric renal or intensive care team. Transfer to tertiary centre
Resonium
Mild effect, multiple doses necessary, may be used as long term agent
- Polystyrene sulfonate (resonium) 0.3-1 g/kg 6 hourly (max 15-30 g) PR or oral (with lactulose)
Note: NOT to be used if ileus, recent abdominal surgery, perforation, hypernatraemia
Onset of Action: 1 hour PR, 4-6 hours oral
Duration: variable
Consider consultation with local paediatric team
-
Any child with moderate or severe hyperkalaemia
- Underlying medical cause - eg renal abnormalities
When to consider transfer to tertiary centre
-
Any child with severe hyperkalaemia
- Any child requiring dialysis
- Child requiring care beyond the comfort level of the hospital
For emergency advice and paediatric or neonatal ICU transfers, call the Paediatric Infant Perinatal Emergency Retrieval (PIPER) Service: 1300 137 650.
Information Specific for RCH
Consider early ICU review if severe hyperkalaemia
Notify child's home team (especially Renal) |
Last updated March 2016