See also
Emergency airway management
Upper airway obstruction
Resuscitation: hospital management of cardiopulmonary arrest
Foreign body ingestion
Key points
- Inhalation of a foreign body (FB) into the trachea or larynx is a potentially life-threatening event requiring immediate emergency airway management
- FB inhalation is frequently unwitnessed and so a high degree of suspicion is required in young children with respiratory symptoms
- A history of inhalation or choking must specifically be sought by clinicians, and may have occurred days or weeks before presentation with symptoms
- A normal respiratory examination or chest x-ray does not exclude an inhaled FB
Background
- The signs and symptoms of FB inhalation will vary depending upon the site of impaction, degree of blockage and type of object
- The vast majority of FB inhalation events occur in children under 4 years and are commonly due to nuts, raw carrot or apple, seeds, popcorn, coins, balloons and pieces of toys. Older children with developmental impairment may continue to be at risk
- Button batteries are more commonly ingested than inhaled, but recognition and management is critical
- Most inhaled FB are located in the bronchi rather than the larynx or trachea
- Children may present with symptoms days to weeks after FB inhalation
Assessment
History
- Detailed description of timing, nature of event and possible FB inhaled, if witnessed
- The site of impaction may be suggested by the clinical presentation
Clinical features based on impaction location
Impaction in larynx or trachea
- Sudden and catastrophic event
- Coughing, choking ± vomiting
- Severe respiratory distress
- Stridor
- Cyanosis
- Altered mental state
- Drooling and voice changes
- Total obstruction will rapidly progress to unconsciousness and cardiorespiratory arrest
- May be present in a child in cardiorespiratory arrest who is impossible to ventilate
|
Impaction in main bronchus
- Witnessed episode of choking, coughing or wheezing while eating or playing (many are unwitnessed)
- Tachypnoea and respiratory distress
- Cyanosis
- Persistent wheeze (may be focal and partially respond to bronchodilators)
- Persistent cough
- Fever
- Haemoptysis
- Shortness of breath
- Recurrent or persistent consolidation
- May be asymptomatic after initial event before developing complications (pneumonia, abscess, bronchiectasis etc)
|
Impaction lower than main bronchus
- Often asymptomatic after initial event, or may have symptoms as for main bronchus FB
|
Examination
- Examination may be normal
- Observe (and maintain) child’s preferred position eg sniffing or tripod
- Work of breathing
- Stridor
- Drooling and altered voice quality
- Asymmetrical chest movement
- Tracheal deviation
- Focal wheeze or decreased breath sounds
- Check for other FB in ears, nose and throat (if child is stable)
Management
If required provide emergency resuscitation prior to other management. Ongoing close observation is required in all children until FB removed, as any movement of FB may cause sudden airway compromise
Investigations
- Normal CXR does not exclude FB inhalation as there may not be signs of air trapping, and most commonly inhaled objects are radiolucent
- Consider CXR ± inspiratory and expiratory films (in children able to cooperate) or lateral decubitus views
- Check for:
- Radio-opaque foreign body
- Segmental or lobar collapse
- Hyperinflation distal to obstruction causing air trapping
- Mediastinal shift
- Consolidation suggestive of pneumonia
- Pneumothorax
- Pulmonary abscess and bronchiectasis are signs of a chronic impacted FB
- CT is not recommended as bronchoscopy is likely to be required; seek expert advice
Treatment
Emergency management
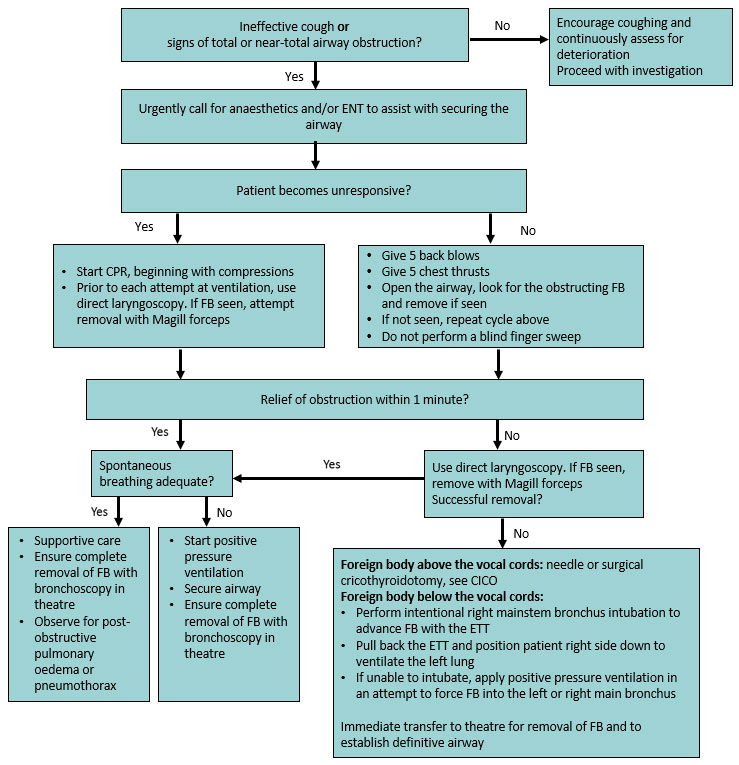
- Attempts at removal of a FB +/- advanced airway management using laryngoscopy, Magill forceps, cricothyroidotomy and other procedures in the flowchart should ideally be performed by a clinician familiar with their use. However, it may be reasonable for a less experienced clinician to proceed if a child is deteriorating.
- If it is not felt to be safe to attempt these procedures, basic resuscitation should be continued while awaiting senior assistance
Subacute management
- In children who have a stable airway where there is ongoing suspicion of an inhaled FB after history and assessment, refer to ENT or respiratory team for consideration of bronchoscopy
- Maintain a high index of suspicion with a low threshold for consultation
Consider consultation with local paediatric team when
A secondary consultation may assist before speciality review
Consider consultation with ENT or respiratory team when
Any suspicion for inhaled FB
Consider transfer when
Local services unable to perform procedures or investigations
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
FB removed and/or child stable after period of observation
Parent information
Prevention strategies:
- Children aged under 5 years are at the greatest risk of inhaled foreign bodies, especially food
- Young children should not be offered hard round foods such as popcorn, hard lollies, uncut grapes, peanuts or other nuts, raw carrot or apples
- Encourage children to always sit calmly while eating, and offer food one piece at a time
- Avoid toys with small parts for children under the age of 3 years
Choking, suffocation and strangulation prevention handout
Last updated March 2021