See also
Anaphylaxis
Asthma
Eczema
Urticaria
Key points
- Recognition and management of anaphylaxis is the most important consideration in any child presenting with suspected food allergy
- A comprehensive history is key to distinguishing true allergy from other types of adverse food reaction
- A child must avoid food(s) suspected of causing an IgE-mediated reaction, but not similar foods that have previously been tolerated
- A child presenting with suspected food allergy should go home with an allergy action plan and appropriate follow-up
Background
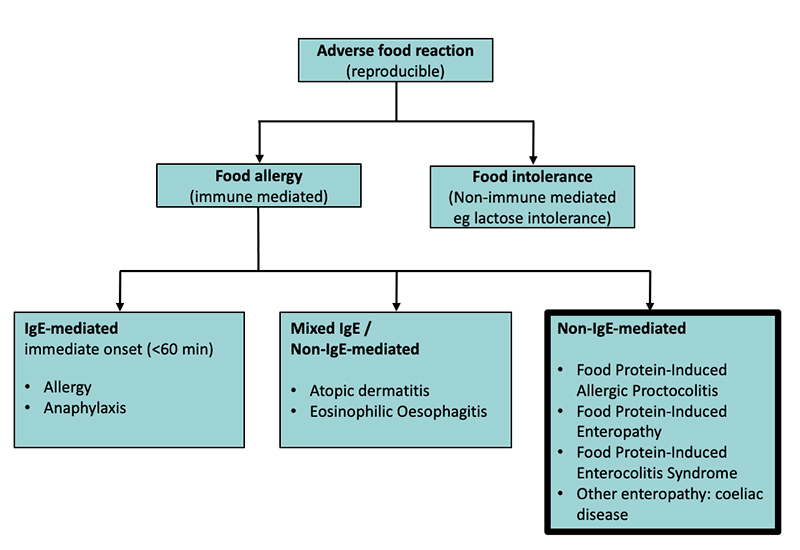
- Food allergies are mediated through the immune system and can be classified as IgE-mediated, non-IgE-mediated, or mixed IgE/non-IgE-mediated
- IgE-mediated reactions are characterized by stereotypical signs and symptoms that develop usually within 60 minutes of ingestion
- The commonest foods implicated in IgE-mediated allergy are peanut, tree nuts, shellfish, fish, milk, egg, wheat, soy, and sesame
- Mild to moderate allergic reactions may involve only skin and/or gastrointestinal symptoms
- Anaphylaxis is any acute onset of respiratory and/or cardiovascular symptoms, even if skin symptoms are not present, and may be life threatening
- Children with IgE-mediated food allergy frequently have other atopic disease, such as asthma, eczema and allergic rhinitis
- Allergy testing is not necessary and is not indicated for suspected non IgE-mediated food allergies, eg non-IgE cow-milk allergy and FPIES (see flowchart below)
Assessment
The goal of assessment is to identify children who present with signs and symptoms of an immediate reaction (see anaphylaxis), as well as those who are clinically well but have a history of possible food allergy
Further assessment should focus on differentiating the clinical features of an IgE-mediated reaction from non-IgE-mediated reactions or food intolerance, and then referring as appropriate
History
- Timing of reaction in relation to food ingestion
- Duration of symptoms
- Exact foods eaten, how much and in what form (eg raw, cooked)
- Other foods ingested at the time
- Age when symptoms first occurred and frequency of occurrence
- Reproducibility on repeat exposures
- Details of previous treatment (eg antihistamines) and response
IgE-mediated food reactions usually occur within 60 minutes of exposure and involve any of the following:
- Skin:
- Rash (eg urticaria)
- Erythema
- Angioedema
- Localised to area of contact (eg perioral) or widespread
- Gastrointestinal tract:
- Abdominal pain
- Nausea or vomiting
- Diarrhoea
- Respiratory:
- Hoarse voice, tightness in throat, difficulty swallowing, stridor
- Wheeze, chest tightness, difficulty breathing, persistent coughing
- Cardiovascular:
- Pallor
- Dizziness, collapse
Risk factors for development of IgE-mediated food allergy
- Personal history of atopy (asthma, eczema or allergic rhinitis)
- History of atopy or food allergy in parents or siblings
- Known other IgE-mediated food allergies
Examination
Acute presentation (see anaphylaxis)
- Airway – hoarseness, stridor, tongue swelling, laryngeal oedema
- Breathing – tachypnoea, cough, wheeze
- Circulation – tachycardia, hypotension
- Skin – rashes, urticaria and angioedema
Differential diagnosis
- Contact skin reaction – erythema and/or urticaria occurring on any areas of skin in contact with the food, more commonly around a child’s mouth. Common in children with eczema and not diagnostic of IgE-mediated food allergy
- Intercurrent illness
- Eczema – eczema alone is not indicative of an immediate IgE-mediated food allergy
- Food Protein Induced Enterocolitis Syndrome (FPIES) – profuse vomiting +/- diarrhoea occurring two to four hours after ingestion of a recently-introduced food. Sometimes associated with pallor, poor tone, a drop in body temperature and low blood pressure. FPIES is non-IgE mediated
Management
Investigations
- Investigations for food allergy are neither necessary nor interpretable in the acute setting
- Diagnosis of food allergy requires convincing history and is supported by Skin Prick Testing (SPT) and specific IgE tests, both of which can be performed after the event
- No investigations are required if the cause of the suspected allergic reaction is unclear
- Skin Prick Testing (SPT) is preferred for suspected IgE allergy, but should only be performed by a paediatric allergy-trained clinician
- If there is no access to an allergy-trained clinician, serum specific IgE testing may be performed. Targeted testing for only the specific suspected food trigger(s) is recommended
- Food allergen screening panels or screening for foods a child has not yet ingested are not recommended, as this can lead to unnecessary food allergen avoidance and greater risk of future food allergies
Treatment
Immediate Management:
- If severe allergic reaction to food, consistent with anaphylaxis:
- Immediately administer Intramuscular Adrenaline, 10 microgram/kg or 0.01 mL/kg of 1:1000 (maximum 0.5 mL)
- Repeat after 5 minutes if not improving
- Refer to Anaphylaxis guideline
- If mild-moderate allergic to reaction, administer a non-sedative antihistamine, eg:
- Cetirizine:
- 1–2 years – 2.5 mg oral
- 2–6 years – 5 mg oral
- 6 years and above – 10 mg oral
- Note: cetirizine has been shown to be safe in infants from 6 months of age (0.25 mg/kg/dose)
Or
- Loratadine:
- 1–2 years, oral 2.5 mg once daily
- >2 years and <30 kg, oral 5 mg once daily
- >30 kg, oral 10 mg once daily
Observe to make sure symptoms do not escalate, then discharge with plan below
Consider discharge when
A plan is provided that addresses the following:
- Strict avoidance of suspected food allergen(s):
- requires parental education on reading ingredient labels (ASCIA Dietary avoidance handouts)
- specific advice for suspected tree-nut allergies:
- if reacted to walnuts, avoid pecans and vice-versa
- if reacted to cashews, avoid pistachios and vice-versa
- Allergy action plan: (Give plan even if food not yet confirmed by investigation)
- Further dietary advice
- Ensure child continues to eat a varied diet, which includes other allergenic foods/nuts that were previously tolerated on a regular basis.
- consider dietician referral if many foods being eliminated, especially if staple foods (eg wheat, milk)
Consider consultation with local paediatric/allergy team when
- Any child with suspected or proven anaphylaxis to a food
- Child with suspected allergy and unstable asthma
- Unclear food trigger or equivocal investigations
- Multiple food allergies
- Suspected tolerance to food on follow-up and which may require an Oral Food Challenge
Parent information
Additional notes
Long-term follow-up
- Regular education on allergy management plan, including checking adrenaline auto-injector technique if child has anaphylaxis plan
- Adrenaline auto-injectors usually have a 12-month expiry, and ongoing prescriptions can be done via local GP
- 150 mcg if child is under 20 kg
- 300 mcg once child is 20 kg
- 300-500 mcg if child close to 50 kg or above
- Identify and manage any asthma. Poorly controlled asthma is a risk factor for fatal anaphylaxis
Last updated October 2021