Key Points
Why?
- to prevent Transfusion Associated Graft-Versus Host Disease (TA-GVHD)
How?
- by gamma irradiation of cellular blood products
What?
- Cellular blood products (whole blood, red blood cells, platelets, granulocytes)
When?
- Timing of irradiation is important for neonatal and paediatric patients. Irradiation reduces the storage-life of red cells and whole blood.
What is TA-GVHD?
- TA-GVHD occurs when donor lymphocytes from transfused blood engraft in the recipient and cause disease. Typically TA-GVHD occurs 10-14 days post transfusion with clinical features of fever, skin rash, hepatitis, diarrhoea and pancytopenia. It is fatal in more than 90% of cases.
Who is at risk?
- Patients who are immuno-compromised and patients receiving transfusion from a relative (directed donation) are at increased risk of TA-GVHD. TA-GVHD has also been reported rarely in patients with a 'normal' immune system.
Transfusion associated graft versus host disease (TA-GVHD)
TA-GVHD is a rare but usually fatal complication of transfusion. The disease occurs when donor lymphocytes engraft in a susceptible recipient. These donor lymphocytes proliferate and damage target organs, especially bone marrow, skin, liver and gastrointestinal tract. Typically the condition presents 10-14 days after transfusion with rash (erythroderma), pancytopenia and abnormal liver function. There is a longer time between transfusion and presentation in neonates. The mortality rate of TA-GVHD approaches 100%.
The risk with an individual transfusion depends on a number of factors including, the viability of contaminating lymphocytes in the blood product, the susceptibility of the recipient's immune system to their engraftment, and the degree of immunologic disparity between the donor and recipient.
TA-GVHD was originally recognised as a complication of intrauterine transfusion and transfusion to recipients of allogeneic bone marrow transplants. The most commonly reported setting for TA-GVHD is immunocompetent recipients of blood from biologically related (directed) or HLA identical donors.
The main stay of preventing TA-GVHD is gamma irradiation of blood products. Leukocyte depletion using current technology is inadequate for this purpose.
Irradiation of blood products
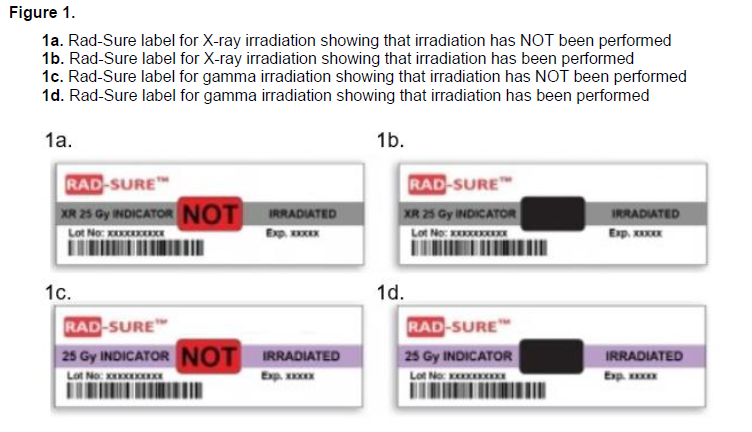
Irradiation of blood products is undertaken using a dedicated blood irradiator located onsite with a long half-life gamma emitting source. Irradiation of blood products will take a further 4 - 5 minutes to provide. If blood products are needed urgently or in the case of an MTP, the products may not be able to be irradiated in a timely manner. Un-irradiated products will be provided in this case. Red cells irradiated at RCH will display the Rad-Sure label for gamma irradiation displayed below.
Irradiation of red blood cells and whole blood results in reduced post transfusion red cell recovery and increases the rate of efflux of intracellular potassium. It has no clinically significant effect on red cell pH, glucose, 2,3 DPG levels or ATP. Packs irradiated within 14 days of collection expire 28 days after collection. Packs irradiated more than 14 days after collection expire either 5 days after irradiation OR at original expiry of pack, whichever comes first. In patients where hyperkalaemia is a concern, red cells should be transfused within 24 hours of irradiation. Examples include large volume neonatal transfusion such as exchange transfusion, ECLS or rapid large volume transfusion.
Irradiation of platelets has not been shown to cause any clinically significant change in platelet function. Platelets may be irradiated at any stage during their 7 day storage life. In Victoria all platelets are irradiated by the Australian Red Cross Lifeblood prior to issue. These products will display the Rad-Sure label for X-RAY irradiation displayed below.
Irradiation of granulocytes. There is conflicting evidence of irradiation damage to granulocytes. Granulocytes should be transfused as soon as possible after collection and irradiation.
Labelling
Blood product irradiation is identified using the Radsure™ system. A label is applied to the blood pack prior to irradiation. The words NOT IRRADIATED are visible. Once irradiation has taken place, the word IRRADIATED remains visible.
Requests
The clinician requesting the crossmatch or blood product is responsible for ensuring irradiated components are requested for appropriate patients. Tick the box on the request form indicating irradiated products are required.
During the final bedside check prior to blood product administration, a check is made to ensure that appropriate blood product modifications such as irradiation has been performed when requested by the treating clinician.
Irradiation Policy at RCH
At RCH a universal blood irradiation policy applies for patients in the following units: PICU, NICU and Children's Cancer Centre. Although not all patients in these units are at risk of TA-GVHD, this policy ensures patients who require irradiated products are not missed.
(Note - haematopoietic stem cells and donor lymphocytes must not be irradiated).
In addition blood is irradiated at RCH in the following circumstances:
- Infants at R.C.H. under 4 months of age
- Cardiac patients with potential T-cell immunodeficiecy
- Immuno-compromised patients i.e.
3.1. Severe Combined Immune Deficiency (SCID), Common Variable Immune Deficiency (CVID)
3.2. Malignancy
3.3. Transplant recipients (bone marrow)
3.4. Haematology/Oncology patients - Neonatal exchange transfusions
- Directed donations
It is the clinicians responsibility to ensure that accurate clinical information is included on orders placed for red cell transfusion or is communicated to the blood bank.